Sunday Poster Session
Category: Interventional Endoscopy
P1111 - A Rare Case of a Duodenal Gangliocytic Paraganglioma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Anila Vasireddy, MD
University of Pennsylvania Health System
Philadelphia, PA
Presenting Author(s)
Anila Vasireddy, MD1, Ali Ismail, MD2, Michael Demarco, DO2, Veena Madhu, MD2, Hiba Hameed Chagla, MD2
1University of Pennsylvania Health System, Philadelphia, PA; 2Penn Medicine, Philadelphia, PA
Introduction: Duodenal gangliocytic paragangliomas are a very rare type of neuroendocrine tumor that can manifest clinically as nausea, vomiting, early satiety, weight loss, or epigastric pain. Evaluation and management requires a multi-modal approach with an upper endoscopy (EGD), endoscopic ultrasonography (EUS), staging with whole-body scans to rule out metastases.
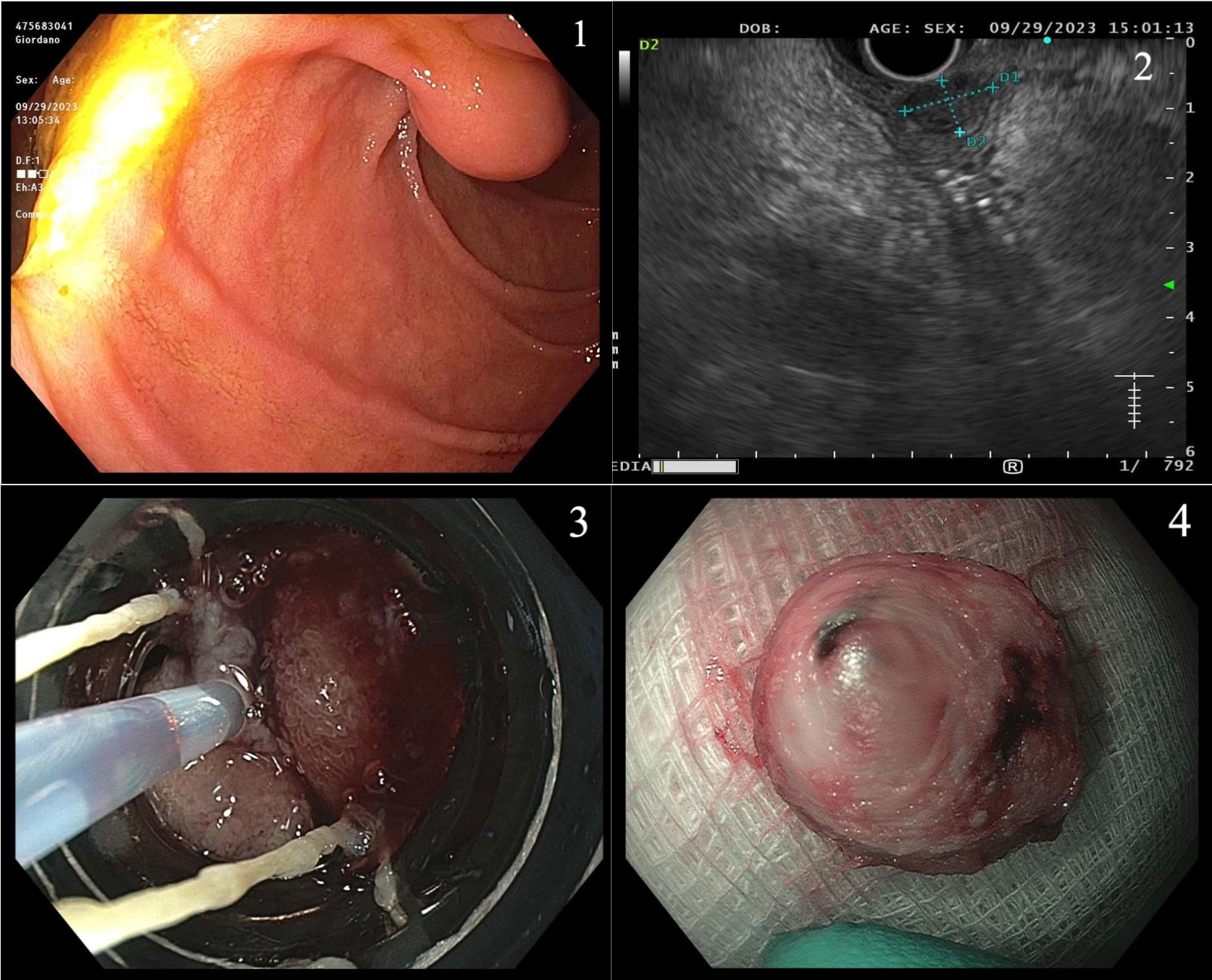
Case Description/Methods: A 67-year-old female with a past medical history of gastroesophageal reflux disease and cirrhosis secondary to MASLD presented with nausea and vomiting. Patient had an upper endoscopy for esophageal variceal screening which demonstrated an incidental subepithelial mass in the 2nd portion of the duodenum. EUS was done which revealed a mass arising from the deep mucosa, 7.2 x 14.2 mm in size, absence of angioinvasion, and initially suggestive of a stromal cell neoplasm. Initially, a trans-duodenal fine needle biopsy was performed which exhibited features of a gangliocytic paraganglioma. A CT/PET dotatate scan was done after which was negative for metastases. Repeat EGD: band ligation and snare mucosal resection was performed to excise the mass. En bloc resection of the mass was carried out with confirmation of complete histologic resection. Patient reported reduction in frequency of nausea and vomiting.
Discussion: Gangliocytic paragangliomas are a type of neuroendocrine tumor which is typically benign. It consists of three components: epithelial, spindle, and ganglion cells. Lymph node metastasis can occur in 5-7% of cases. They can be resected via four methods: endoscopic mucosal resection (EMR), endoscopic mucosal resection with ligation device (EMR-L), endoscopic submucosal resection (ESR) or surgical resection. The resection modality is dependent on the size of the mass, EUS features, presence of angioinvasion, proximity to other vital structures, and endoscopists’ expertise. EMR is associated with shorter scope time and higher rates of complete histologic resection as compared to EMR-L/ESR. ESR has higher rates of successful en bloc resection, but higher rates of complications. EMR-L is indicated for lesions in the deep mucosal/submucosal layer + ≤ 1 cm.
Disclosures:
Anila Vasireddy, MD1, Ali Ismail, MD2, Michael Demarco, DO2, Veena Madhu, MD2, Hiba Hameed Chagla, MD2. P1111 - A Rare Case of a Duodenal Gangliocytic Paraganglioma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania Health System, Philadelphia, PA; 2Penn Medicine, Philadelphia, PA
Introduction: Duodenal gangliocytic paragangliomas are a very rare type of neuroendocrine tumor that can manifest clinically as nausea, vomiting, early satiety, weight loss, or epigastric pain. Evaluation and management requires a multi-modal approach with an upper endoscopy (EGD), endoscopic ultrasonography (EUS), staging with whole-body scans to rule out metastases.
Case Description/Methods: A 67-year-old female with a past medical history of gastroesophageal reflux disease and cirrhosis secondary to MASLD presented with nausea and vomiting. Patient had an upper endoscopy for esophageal variceal screening which demonstrated an incidental subepithelial mass in the 2nd portion of the duodenum. EUS was done which revealed a mass arising from the deep mucosa, 7.2 x 14.2 mm in size, absence of angioinvasion, and initially suggestive of a stromal cell neoplasm. Initially, a trans-duodenal fine needle biopsy was performed which exhibited features of a gangliocytic paraganglioma. A CT/PET dotatate scan was done after which was negative for metastases. Repeat EGD: band ligation and snare mucosal resection was performed to excise the mass. En bloc resection of the mass was carried out with confirmation of complete histologic resection. Patient reported reduction in frequency of nausea and vomiting.
The small intestinal subepithelial biopsy was consistent with a composite gangliocytoma/neuroma and neuroendocrine tumor (CoGNET). Immunohistochemistry (IHC) of the epithelioid cells were positive for synaptophysin, chromogranin, CKIT, PanCK, and AE1/3. IHC of the spindle cells revealed positivity to S100, SOX10, CKIT. Ki67 proliferation index was approximately 1%.
Discussion: Gangliocytic paragangliomas are a type of neuroendocrine tumor which is typically benign. It consists of three components: epithelial, spindle, and ganglion cells. Lymph node metastasis can occur in 5-7% of cases. They can be resected via four methods: endoscopic mucosal resection (EMR), endoscopic mucosal resection with ligation device (EMR-L), endoscopic submucosal resection (ESR) or surgical resection. The resection modality is dependent on the size of the mass, EUS features, presence of angioinvasion, proximity to other vital structures, and endoscopists’ expertise. EMR is associated with shorter scope time and higher rates of complete histologic resection as compared to EMR-L/ESR. ESR has higher rates of successful en bloc resection, but higher rates of complications. EMR-L is indicated for lesions in the deep mucosal/submucosal layer + ≤ 1 cm.
Figure: Figure 1. Mass in the 2nd portion of the duodenum; 2. EUS of the mass; 3. Endoscopic mucosal resection with ligation; 4. En bloc resection of the mass
Disclosures:
Anila Vasireddy indicated no relevant financial relationships.
Ali Ismail indicated no relevant financial relationships.
Michael Demarco indicated no relevant financial relationships.
Veena Madhu indicated no relevant financial relationships.
Hiba Hameed Chagla indicated no relevant financial relationships.
Anila Vasireddy, MD1, Ali Ismail, MD2, Michael Demarco, DO2, Veena Madhu, MD2, Hiba Hameed Chagla, MD2. P1111 - A Rare Case of a Duodenal Gangliocytic Paraganglioma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
