Sunday Poster Session
Category: Interventional Endoscopy
P1114 - Pancreatic Cancer Complicating a Duct Leak Managed by EUS
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Syed Hamza Sohail, MD
University of Massachusetts Chan Medical School - Baystate Health
Springfield, MA
Presenting Author(s)
Syed Hamza Sohail, MD1, Kamesh Gupta, MD2, Syed Hammad Kazmi, MD3, Nha Duong, DO4
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2Baystate Medical Center, Enfield, CT; 3Robert Wood Johnson University Hospital, Bronx, NY; 4University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA
Introduction: Pancreatic duct (PD) leaks are often managed by placement of a PD stent via endoscopic retrograde pancreatography (ERP) approach. However, the PD cannot be accessed in 3-10% of cases due to obstruction, typically from a tumor. Endoscopic ultrasound (EUS) guided pancreaticogastrostomy (PG) can help achieve access to the PD for therapeutic purposes. We describe a case of a post splenectomy tail leak that was complicated by a head of pancreas (HOP) tumor managed by an EUS-PG.
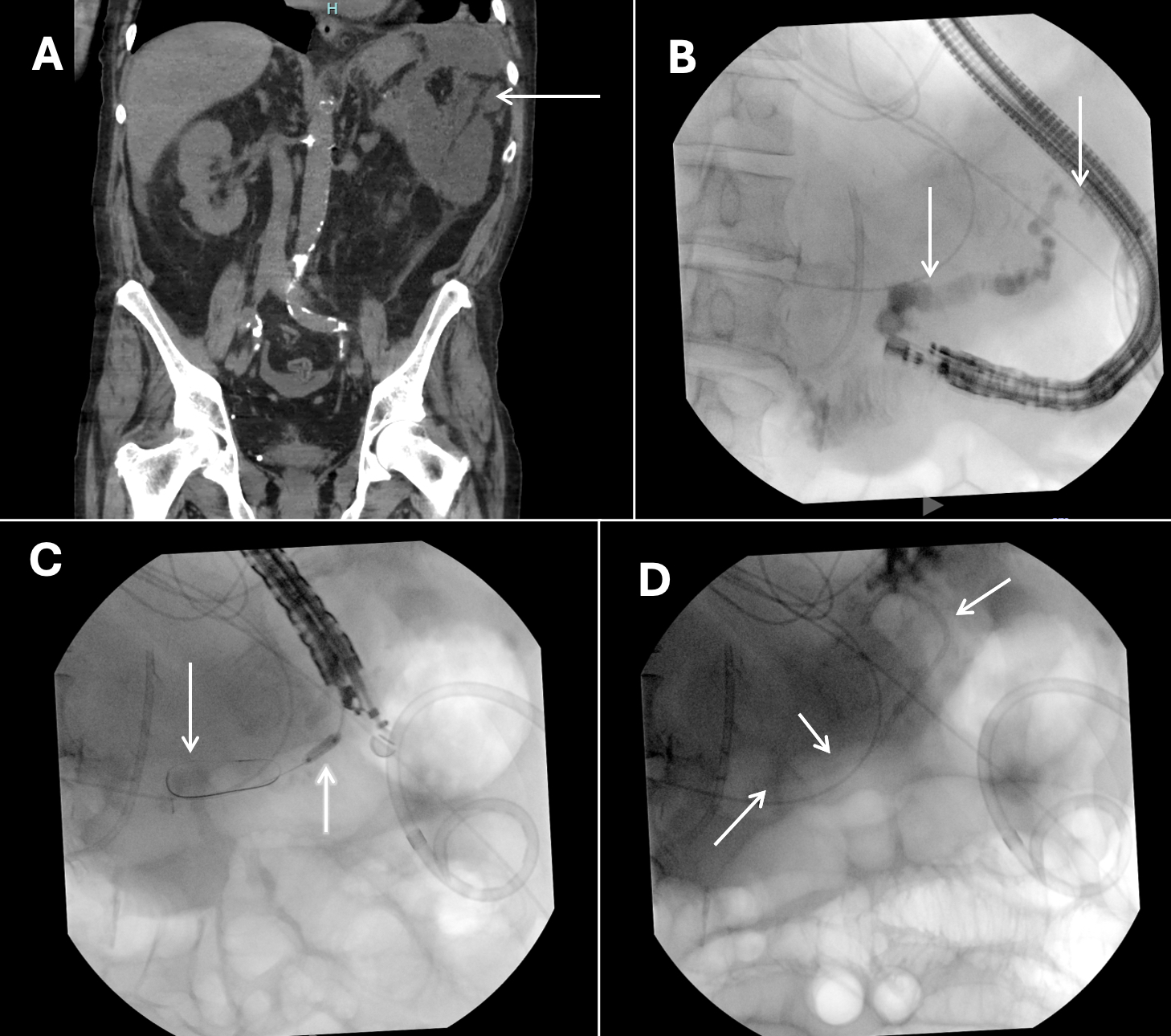
Case Description/Methods: 74-year-old male with known HOP adenocarcinoma causing upstream PD dilatation developed a recent traumatic splenic injury requiring emergent splenectomy. Soon afterwards the patient presented to the hospital with left sided abdominal pain. Cholestatic LFT elevation pointed to biliary obstruction due to the HOP mass. Imaging was also concerning for a 7.3cm fluid collection in splenic fossa. A CT guided drain was placed, and fluid studies revealed an amylase of 14,718 and a lipase of >15,000. This was consistent with a PD leak precipitated by the splenectomy but worsened by the downstream obstruction in the HOP. He underwent ERCP with successful biliary stent placement however we failed to deeply cannulate the PD due to the obstructing tumor with a very narrow stricture.
We attempted EUS several days later. MPD was punctured from the duodenum under EUS guidance and a pancreatogram revealed a large caliber leak in the tail. The contrast drained into the area of IR catheter. We initially attempted antegrade access for a potential rendezvous ERP but this was unsuccessful.
PG was then pursued for internal drainage of MPD into the stomach. A 0.025" wire was left in place within the PD. A 4 mm biliary dilation balloon was used to dilate the tract over the wire and then a 7Fr x 3cm double pigtail stent was placed draining into the gastric body. The IR drain was clamped and repeat imaging 3 days later showed dramatic decrease in the fluid collection demonstrating good internal drainage. The patient continued to do well 2 weeks later, and the IR drain was removed.
Discussion: EUS-guided interventions are effective alternatives when traditional approaches are unsuccessful. Our case is a rare instance where a splenectomy without distal pancreatectomy resulted in a PD leak. This was likely precipitated by elevated pressures in the PD system due to the downstream tumor causing obstruction. Our case demonstrates how EUS can be safely used to manage PD leaks and pancreatic fluid collections in a less invasive manner.
Disclosures:
Syed Hamza Sohail, MD1, Kamesh Gupta, MD2, Syed Hammad Kazmi, MD3, Nha Duong, DO4. P1114 - Pancreatic Cancer Complicating a Duct Leak Managed by EUS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2Baystate Medical Center, Enfield, CT; 3Robert Wood Johnson University Hospital, Bronx, NY; 4University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA
Introduction: Pancreatic duct (PD) leaks are often managed by placement of a PD stent via endoscopic retrograde pancreatography (ERP) approach. However, the PD cannot be accessed in 3-10% of cases due to obstruction, typically from a tumor. Endoscopic ultrasound (EUS) guided pancreaticogastrostomy (PG) can help achieve access to the PD for therapeutic purposes. We describe a case of a post splenectomy tail leak that was complicated by a head of pancreas (HOP) tumor managed by an EUS-PG.
Case Description/Methods: 74-year-old male with known HOP adenocarcinoma causing upstream PD dilatation developed a recent traumatic splenic injury requiring emergent splenectomy. Soon afterwards the patient presented to the hospital with left sided abdominal pain. Cholestatic LFT elevation pointed to biliary obstruction due to the HOP mass. Imaging was also concerning for a 7.3cm fluid collection in splenic fossa. A CT guided drain was placed, and fluid studies revealed an amylase of 14,718 and a lipase of >15,000. This was consistent with a PD leak precipitated by the splenectomy but worsened by the downstream obstruction in the HOP. He underwent ERCP with successful biliary stent placement however we failed to deeply cannulate the PD due to the obstructing tumor with a very narrow stricture.
We attempted EUS several days later. MPD was punctured from the duodenum under EUS guidance and a pancreatogram revealed a large caliber leak in the tail. The contrast drained into the area of IR catheter. We initially attempted antegrade access for a potential rendezvous ERP but this was unsuccessful.
PG was then pursued for internal drainage of MPD into the stomach. A 0.025" wire was left in place within the PD. A 4 mm biliary dilation balloon was used to dilate the tract over the wire and then a 7Fr x 3cm double pigtail stent was placed draining into the gastric body. The IR drain was clamped and repeat imaging 3 days later showed dramatic decrease in the fluid collection demonstrating good internal drainage. The patient continued to do well 2 weeks later, and the IR drain was removed.
Discussion: EUS-guided interventions are effective alternatives when traditional approaches are unsuccessful. Our case is a rare instance where a splenectomy without distal pancreatectomy resulted in a PD leak. This was likely precipitated by elevated pressures in the PD system due to the downstream tumor causing obstruction. Our case demonstrates how EUS can be safely used to manage PD leaks and pancreatic fluid collections in a less invasive manner.
Figure: Figure A: Fluid collection in splenic fossa.
Figure B: Pancreatogram with arrows showing dilated PD and the leak in the tail.
Figure C: Arrows point to the coiled wire in PD and a 4mm balloon being used to dilate the tract.
Figure D: Arrows point to the 7 French double pigtail stent in the PD with one end in the stomach.
Figure B: Pancreatogram with arrows showing dilated PD and the leak in the tail.
Figure C: Arrows point to the coiled wire in PD and a 4mm balloon being used to dilate the tract.
Figure D: Arrows point to the 7 French double pigtail stent in the PD with one end in the stomach.
Disclosures:
Syed Hamza Sohail indicated no relevant financial relationships.
Kamesh Gupta indicated no relevant financial relationships.
Syed Hammad Kazmi indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Syed Hamza Sohail, MD1, Kamesh Gupta, MD2, Syed Hammad Kazmi, MD3, Nha Duong, DO4. P1114 - Pancreatic Cancer Complicating a Duct Leak Managed by EUS, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
