Sunday Poster Session
Category: Interventional Endoscopy
P1120 - Unraveling the Enigma: A Case Study on Gastric Schwannoma and it's Clinical Implications
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kelsey Lamb, DO
HCA Florida Largo Hospital
Clearwater, FL
Presenting Author(s)
Kelsey Lamb, DO1, Suhail Kayyali, DO2, Michael Schulman, DO2, Meir Mizrahi, MD2
1HCA Florida Largo Hospital, Clearwater, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Gastrointestinal schwannoma (GIS) represents a rare subset of gastrointestinal (GI) neoplasms. Distinguishing these tumors from other mesenchymal lesions, such as gastrointestinal stromal tumors (GISTs), is crucial for appropriate management. This case study explores the clinical journey of a patient diagnosed with a gastric schwannoma, shedding light on the challenges in diagnosis and variance in treatment.
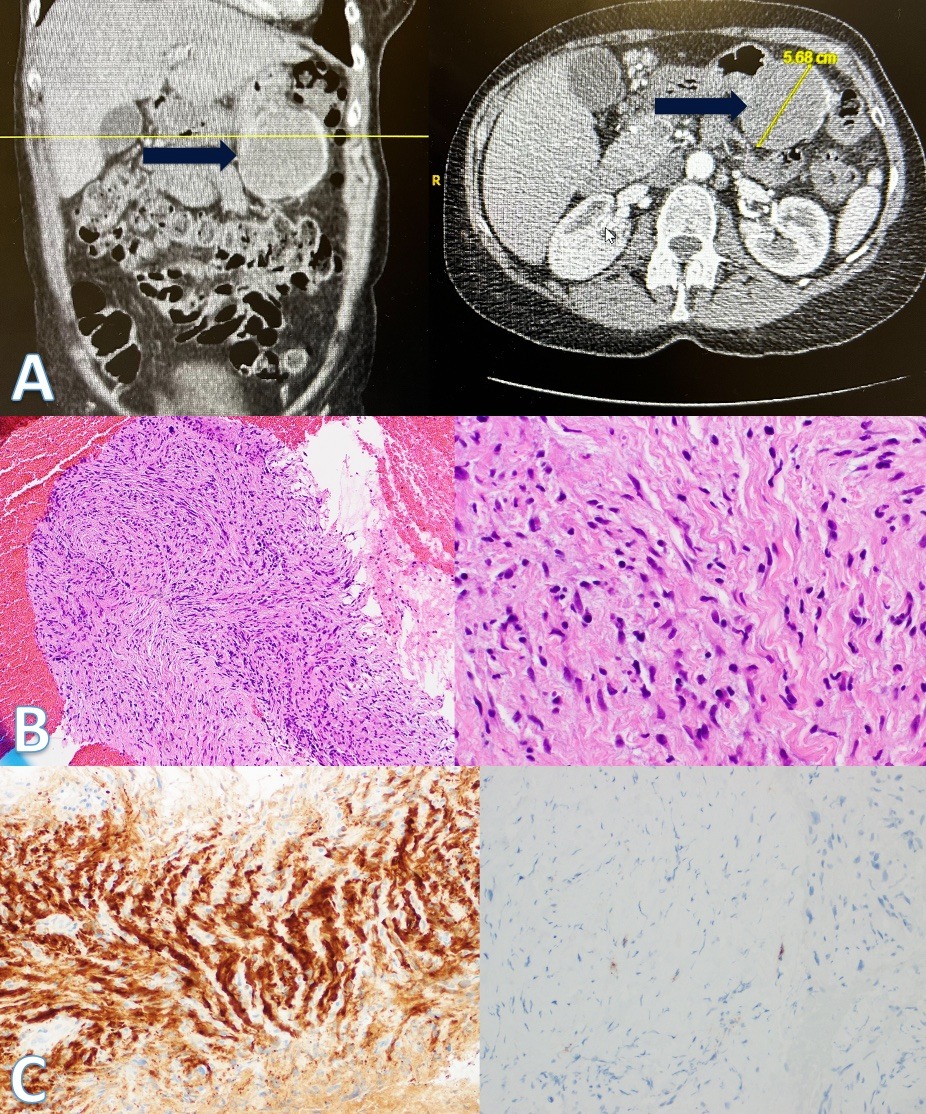
Case Description/Methods: A 67-year-old female presented to the outpatient GI office for initial evaluation of an incidental gastric lesion. Computed tomography angiography (CTA) of the chest/abdomen/pelvis revealed an incidental gastric mass, concerning for GIST. The patient had no prior esophagogastroduodenoscopy (EGD) or colonoscopy. She denied any GI symptoms at that time.
EUS was performed and showed an exophytic, ill-defined, gastric mass in the body of the stomach. The lesion measured 6.9 cm x 6.0 cm. The lesion was heterogenous in echotexture. The borders of the mass were irregular and poorly defined making it difficult to differentiate the layer of origin. Fine needle biopsies of the mass were obtained and sent for histopathologic analysis with findings consistent with schwannoma.
Discussion: Schwannomas are slow-growing, often benign tumors originating from mesenchymal stem cells. GIS is an extremely rare neoplasm and accounts for approximately 0.2% of all gastric malignancies.
Diagnosing GIS can be challenging due to its rarity and the similarity of symptoms to other gastrointestinal conditions. Imaging studies, such as CT scans and endoscopy are done initially; however, immunohistochemical testing is required for definitive diagnosis. Histologic features typically display spindle cells with focal nuclear atypia. Immunohistochemical testing is required for definitive diagnosis of GIS and this includes staining positive for S-100 and negative for CD117. On the contrary, GISTs, the most common mesenchymal GI tumor, stain negative for S-100 and positive for CD117. Prior to the identification of S-100, schwannomas were often misdiagnosed.
Management of GIS usually involves surgical resection, and the prognosis is generally favorable for benign cases. Although rare, malignant transformation carries a poor prognosis and may require additional treatments, such as chemotherapy. As research on gastric schwannomas is ongoing, further understanding of its pathogenesis and optimal treatment approaches will likely emerge.
Disclosures:
Kelsey Lamb, DO1, Suhail Kayyali, DO2, Michael Schulman, DO2, Meir Mizrahi, MD2. P1120 - Unraveling the Enigma: A Case Study on Gastric Schwannoma and it's Clinical Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Florida Largo Hospital, Clearwater, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Gastrointestinal schwannoma (GIS) represents a rare subset of gastrointestinal (GI) neoplasms. Distinguishing these tumors from other mesenchymal lesions, such as gastrointestinal stromal tumors (GISTs), is crucial for appropriate management. This case study explores the clinical journey of a patient diagnosed with a gastric schwannoma, shedding light on the challenges in diagnosis and variance in treatment.
Case Description/Methods: A 67-year-old female presented to the outpatient GI office for initial evaluation of an incidental gastric lesion. Computed tomography angiography (CTA) of the chest/abdomen/pelvis revealed an incidental gastric mass, concerning for GIST. The patient had no prior esophagogastroduodenoscopy (EGD) or colonoscopy. She denied any GI symptoms at that time.
EUS was performed and showed an exophytic, ill-defined, gastric mass in the body of the stomach. The lesion measured 6.9 cm x 6.0 cm. The lesion was heterogenous in echotexture. The borders of the mass were irregular and poorly defined making it difficult to differentiate the layer of origin. Fine needle biopsies of the mass were obtained and sent for histopathologic analysis with findings consistent with schwannoma.
Discussion: Schwannomas are slow-growing, often benign tumors originating from mesenchymal stem cells. GIS is an extremely rare neoplasm and accounts for approximately 0.2% of all gastric malignancies.
Diagnosing GIS can be challenging due to its rarity and the similarity of symptoms to other gastrointestinal conditions. Imaging studies, such as CT scans and endoscopy are done initially; however, immunohistochemical testing is required for definitive diagnosis. Histologic features typically display spindle cells with focal nuclear atypia. Immunohistochemical testing is required for definitive diagnosis of GIS and this includes staining positive for S-100 and negative for CD117. On the contrary, GISTs, the most common mesenchymal GI tumor, stain negative for S-100 and positive for CD117. Prior to the identification of S-100, schwannomas were often misdiagnosed.
Management of GIS usually involves surgical resection, and the prognosis is generally favorable for benign cases. Although rare, malignant transformation carries a poor prognosis and may require additional treatments, such as chemotherapy. As research on gastric schwannomas is ongoing, further understanding of its pathogenesis and optimal treatment approaches will likely emerge.
Figure: A: CT of the abdomen/pelvis showed a 5.5 cm gastric lesion, concerning for GIST (arrows). B: Low power histological view showing spindle cell neoplasia (left). High power histological image displaying cells with two pointed ends consistent with neural tissue (right). C: Staining positive for S100 consistent with neuroectoderm lineage (left). CD117 negative ruling out GIST (right).
Disclosures:
Kelsey Lamb indicated no relevant financial relationships.
Suhail Kayyali indicated no relevant financial relationships.
Michael Schulman indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Kelsey Lamb, DO1, Suhail Kayyali, DO2, Michael Schulman, DO2, Meir Mizrahi, MD2. P1120 - Unraveling the Enigma: A Case Study on Gastric Schwannoma and it's Clinical Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
