Sunday Poster Session
Category: Liver
P1192 - Understanding the Role of Obesity in Alcoholic Hepatitis: Findings from a National Cohort
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ali Jaan, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Mostafa Najim, MD2, Ashish Dhawan, MBBS3, Umer Farooq, MD4, Laraib Fatima. Sheikh, 5, Sushil Ahlawat, MD, MS, MBBS6
1Rochester General Hospital, Rochester, NY; 2Unity Hospital, Rochester, NY; 3Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5Lahore Medical and Dental College, Rochester, NY; 6SUNY Downstate Health Sciences University, Brooklyn, NY
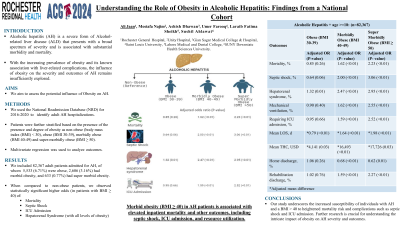
Introduction: Alcoholic hepatitis (AH) represents a severe manifestation of alcoholic liver disease characterized by acute-onset inflammation and liver dysfunction. It presents a wide severity spectrum, from self-limiting disease to severe cases associated with a high mortality risk. With the increasing prevalence of obesity and its known association with liver-related complications, this study aims to investigate the influence of obesity on the severity and outcomes of AH.
Methods: Using the National Readmission Database (NRD) 2016-2020, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients admitted with AH. We further classified AH patients based on the presence and degree of obesity as non-obese (body mass index (BMI) < 30), obese (BMI 30-39), morbidly obese (BMI 40-49) and super-morbidly obese (BMI ≥ 50). Using a multivariate regression model, we compared the outcomes of AH hospitalizations. STATA 14.2 was utilized for statistical analysis.
Results: We included 82,367 AH patients, of whom 5,533 (6.71%) were obese, 2,606 (3.16%) had morbid obesity, and 633 (0.77%) had super morbid obesity (Table 1). When compared to non-obese patients, we observed significantly elevated odds of mortality in both morbidly obese and super-morbidly obese subgroups (adjusted odds ratios (aOR) 1.62 & 2.23 respectively, P< 0.01). Patients with a BMI > 40 had higher odds of complications, including septic shock and intensive care unit (ICU) admission (P< 0.01). Additionally, AH-specific complication, i.e., hepatorenal syndrome (HRS), exhibited elevated odds for all levels of obesity. No statistically significant difference was observed in the odds of spontaneous bacterial peritonitis or variceal upper gastrointestinal bleeding. Resource utilization also demonstrated a progressive increase with increasing severity of obesity (P≤0.03).
Discussion: Our study underscores the increased susceptibility of individuals with AH and a BMI exceeding 40 to heightened mortality risk and complications such as septic shock and ICU admission. The likelihood of HRS and the utilization of hospital resources escalates in tandem with the severity of obesity. Further research is crucial for a comprehensive understanding of the intricate impact of obesity on AH severity and outcomes. This knowledge will inform better clinical management and resource allocation across diverse healthcare settings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan, MD1, Mostafa Najim, MD2, Ashish Dhawan, MBBS3, Umer Farooq, MD4, Laraib Fatima. Sheikh, 5, Sushil Ahlawat, MD, MS, MBBS6. P1192 - Understanding the Role of Obesity in Alcoholic Hepatitis: Findings from a National Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Unity Hospital, Rochester, NY; 3Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5Lahore Medical and Dental College, Rochester, NY; 6SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Alcoholic hepatitis (AH) represents a severe manifestation of alcoholic liver disease characterized by acute-onset inflammation and liver dysfunction. It presents a wide severity spectrum, from self-limiting disease to severe cases associated with a high mortality risk. With the increasing prevalence of obesity and its known association with liver-related complications, this study aims to investigate the influence of obesity on the severity and outcomes of AH.
Methods: Using the National Readmission Database (NRD) 2016-2020, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients admitted with AH. We further classified AH patients based on the presence and degree of obesity as non-obese (body mass index (BMI) < 30), obese (BMI 30-39), morbidly obese (BMI 40-49) and super-morbidly obese (BMI ≥ 50). Using a multivariate regression model, we compared the outcomes of AH hospitalizations. STATA 14.2 was utilized for statistical analysis.
Results: We included 82,367 AH patients, of whom 5,533 (6.71%) were obese, 2,606 (3.16%) had morbid obesity, and 633 (0.77%) had super morbid obesity (Table 1). When compared to non-obese patients, we observed significantly elevated odds of mortality in both morbidly obese and super-morbidly obese subgroups (adjusted odds ratios (aOR) 1.62 & 2.23 respectively, P< 0.01). Patients with a BMI > 40 had higher odds of complications, including septic shock and intensive care unit (ICU) admission (P< 0.01). Additionally, AH-specific complication, i.e., hepatorenal syndrome (HRS), exhibited elevated odds for all levels of obesity. No statistically significant difference was observed in the odds of spontaneous bacterial peritonitis or variceal upper gastrointestinal bleeding. Resource utilization also demonstrated a progressive increase with increasing severity of obesity (P≤0.03).
Discussion: Our study underscores the increased susceptibility of individuals with AH and a BMI exceeding 40 to heightened mortality risk and complications such as septic shock and ICU admission. The likelihood of HRS and the utilization of hospital resources escalates in tandem with the severity of obesity. Further research is crucial for a comprehensive understanding of the intricate impact of obesity on AH severity and outcomes. This knowledge will inform better clinical management and resource allocation across diverse healthcare settings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Mostafa Najim indicated no relevant financial relationships.
Ashish Dhawan indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Laraib Sheikh indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Ali Jaan, MD1, Mostafa Najim, MD2, Ashish Dhawan, MBBS3, Umer Farooq, MD4, Laraib Fatima. Sheikh, 5, Sushil Ahlawat, MD, MS, MBBS6. P1192 - Understanding the Role of Obesity in Alcoholic Hepatitis: Findings from a National Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
