Sunday Poster Session
Category: Liver
P1221 - Intrahepatic Cholangiocarcinoma Treated With Liver Transplantation: Long Term Outcomes From a Single Transplant Center
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FG
Fernando Gil Lopez, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Fernando Gil Lopez, MD, Lydia A. Mercado, MD, Kristopher Croome, MD, David Lee, MD, Raouf Nakhleh, MD, Denise Harnois, DO
Mayo Clinic, Jacksonville, FL
Introduction: Historically, intrahepatic cholangiocarcinoma (iCCA)had been considered a contraindication for liver transplantation (LT) due to poor outcomes. However, in the last decade, mainly retrospective data from patients with small (≤2 cm), liver-limited iCCA has provided promising results. More recently, transplant for iCCA has become more accepted, however, there is limited data on long term outcomes for these patients.
Methods: A retrospective chart review of patients with an explant-confirmed diagnosis of iCCA or combined iCCA and hepatocellular carcinoma (cCCA-HCC) treated with LT at Mayo Clinic Florida from February 1998 to December 2023 was conducted. Overall, 17 adult patients were included. Descriptive statistics were used. Survival was considered from the day of LT. Overall survival and event free-survival (event was defined as cancer recurrence or death) was estimated using the Kaplan-Meier method. One patient received a simultaneous liver-kidney transplant.
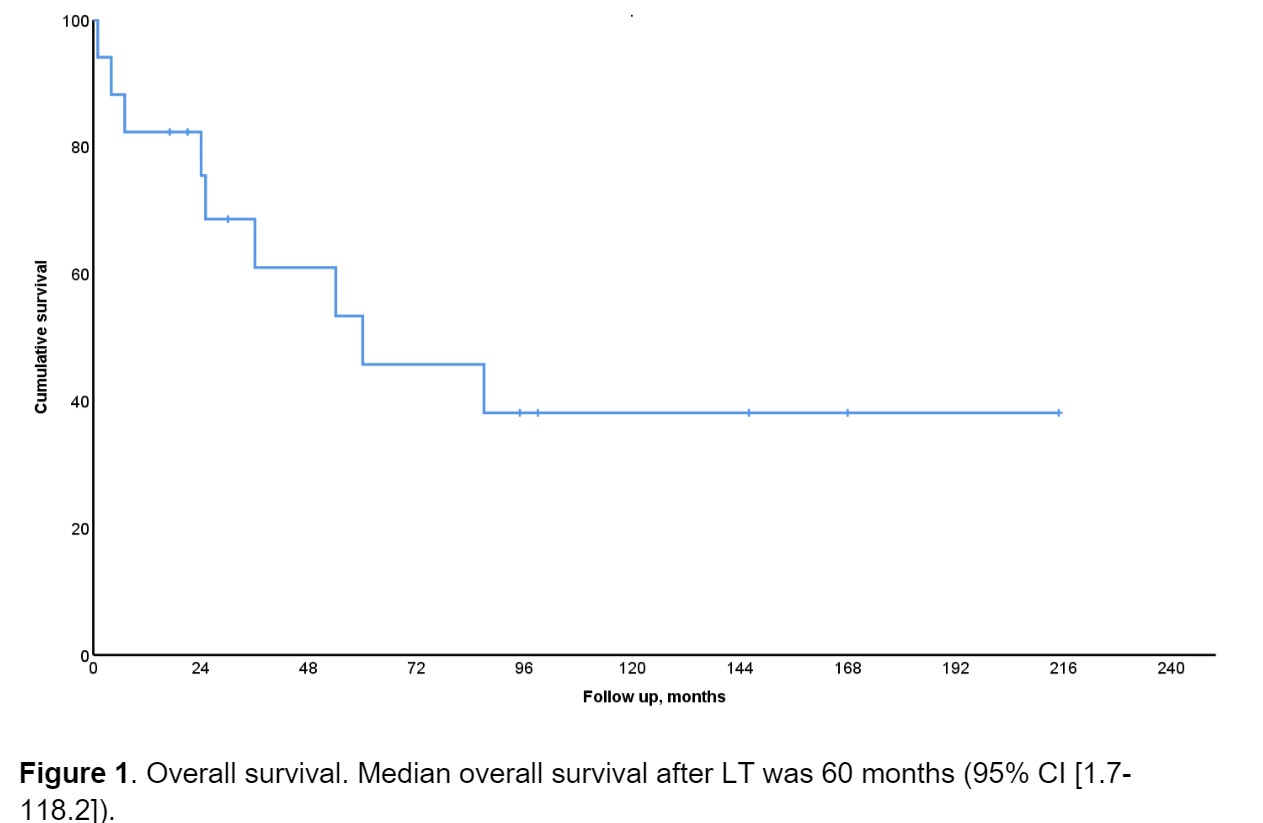
Results: All patients had underlying cirrhosis. 5 cases were incidentally found on explant after LT. Twelve patients had pure iCCA histology on explant, and 5 had cCCA-HCC. 12 patients received locoregional therapy prior to transplant, 12 transarterial chemoembolization, 1 radioembolization, and 1 radiofrequency ablation. Mean Raw-MELD at transplant was 15.7 (6-33). The median time from listing to transplant was 1 month (0-8). The median tumor number on imaging was 1 (0-4). There were no intraoperative deaths, no cases of graft primary non-function, nor graft-failure cases during follow-up. Other relevant variables are included in table 1. Median overall survival after LT was 60 months (95% CI [1.7-118.2]) (Figure 1). Three patients had pulmonary recurrence, 1 had liver and pulmonary recurrence. 5 deaths were related to cancer recurrence, 4 were due to unrelated conditions. Median event-free survival was 61 months (95% CI [0-123.1]).
Discussion: Although limited by a small sample size, our study reinforces LT for iCCA. It may provide a suitable long-term recurrence-free survival and overall survival in the context of low grade, liver-limited, small, solitary iCCA. Thus, in experienced transplant centers and within the appropriate clinical context, neoadjuvant locoregional treatment followed by LT may be considered an acceptable option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fernando Gil Lopez, MD, Lydia A. Mercado, MD, Kristopher Croome, MD, David Lee, MD, Raouf Nakhleh, MD, Denise Harnois, DO. P1221 - Intrahepatic Cholangiocarcinoma Treated With Liver Transplantation: Long Term Outcomes From a Single Transplant Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Historically, intrahepatic cholangiocarcinoma (iCCA)had been considered a contraindication for liver transplantation (LT) due to poor outcomes. However, in the last decade, mainly retrospective data from patients with small (≤2 cm), liver-limited iCCA has provided promising results. More recently, transplant for iCCA has become more accepted, however, there is limited data on long term outcomes for these patients.
Methods: A retrospective chart review of patients with an explant-confirmed diagnosis of iCCA or combined iCCA and hepatocellular carcinoma (cCCA-HCC) treated with LT at Mayo Clinic Florida from February 1998 to December 2023 was conducted. Overall, 17 adult patients were included. Descriptive statistics were used. Survival was considered from the day of LT. Overall survival and event free-survival (event was defined as cancer recurrence or death) was estimated using the Kaplan-Meier method. One patient received a simultaneous liver-kidney transplant.
Results: All patients had underlying cirrhosis. 5 cases were incidentally found on explant after LT. Twelve patients had pure iCCA histology on explant, and 5 had cCCA-HCC. 12 patients received locoregional therapy prior to transplant, 12 transarterial chemoembolization, 1 radioembolization, and 1 radiofrequency ablation. Mean Raw-MELD at transplant was 15.7 (6-33). The median time from listing to transplant was 1 month (0-8). The median tumor number on imaging was 1 (0-4). There were no intraoperative deaths, no cases of graft primary non-function, nor graft-failure cases during follow-up. Other relevant variables are included in table 1. Median overall survival after LT was 60 months (95% CI [1.7-118.2]) (Figure 1). Three patients had pulmonary recurrence, 1 had liver and pulmonary recurrence. 5 deaths were related to cancer recurrence, 4 were due to unrelated conditions. Median event-free survival was 61 months (95% CI [0-123.1]).
Discussion: Although limited by a small sample size, our study reinforces LT for iCCA. It may provide a suitable long-term recurrence-free survival and overall survival in the context of low grade, liver-limited, small, solitary iCCA. Thus, in experienced transplant centers and within the appropriate clinical context, neoadjuvant locoregional treatment followed by LT may be considered an acceptable option.
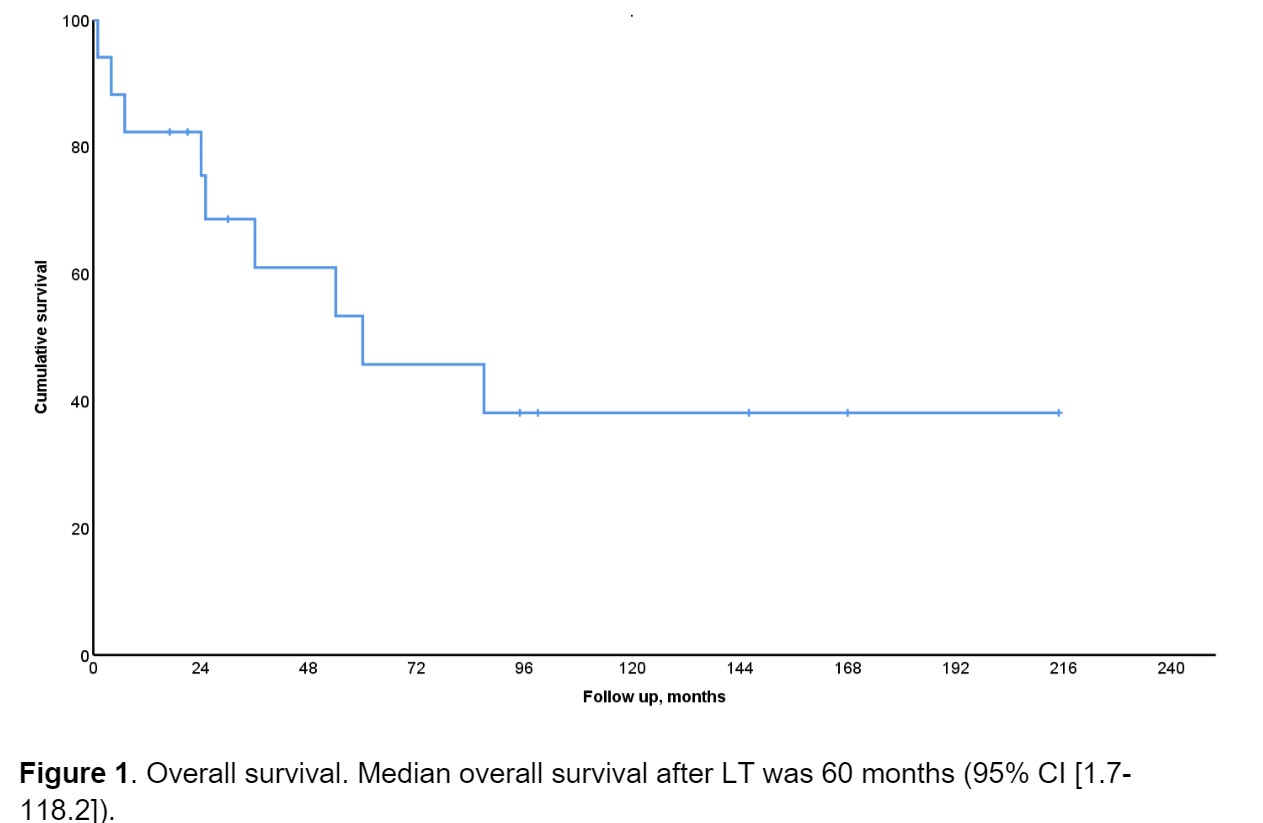
Figure: Figure 1. Overall survival. Median overall survival after LT was 60 months (95% CI [1.7-118.2]).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fernando Gil Lopez indicated no relevant financial relationships.
Lydia Mercado indicated no relevant financial relationships.
Kristopher Croome indicated no relevant financial relationships.
David Lee indicated no relevant financial relationships.
Raouf Nakhleh indicated no relevant financial relationships.
Denise Harnois indicated no relevant financial relationships.
Fernando Gil Lopez, MD, Lydia A. Mercado, MD, Kristopher Croome, MD, David Lee, MD, Raouf Nakhleh, MD, Denise Harnois, DO. P1221 - Intrahepatic Cholangiocarcinoma Treated With Liver Transplantation: Long Term Outcomes From a Single Transplant Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
