Sunday Poster Session
Category: Liver
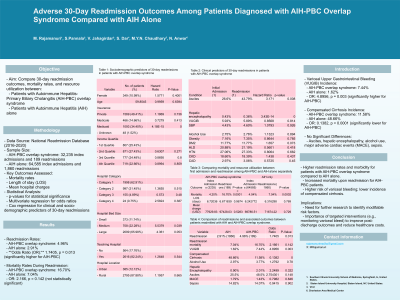
P1250 - Adverse 30-Day Readmission Outcomes Among Patients Diagnosed with AIH-PBC Overlap Syndrome Compared with AIH Alone
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Medha Rajamanuri, MBBS
Southern Illinois University
springfield, IL
Presenting Author(s)
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Vinay Jahagirdar, MD3, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB4, Nadeem Anwar, MD5
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Indiana University Southwest, Evansville, IN; 5West Virginia University Charleston Area Medical Center, Charleston, WV
Introduction: This study aims to compare 30-day readmission outcomes, mortality rates, and resource utilization between patients diagnosed with Autoimmune Hepatitis-Primary Biliary Cholangitis (AIH-PBC) overlap syndrome and those with Autoimmune Hepatitis (AIH) alone.
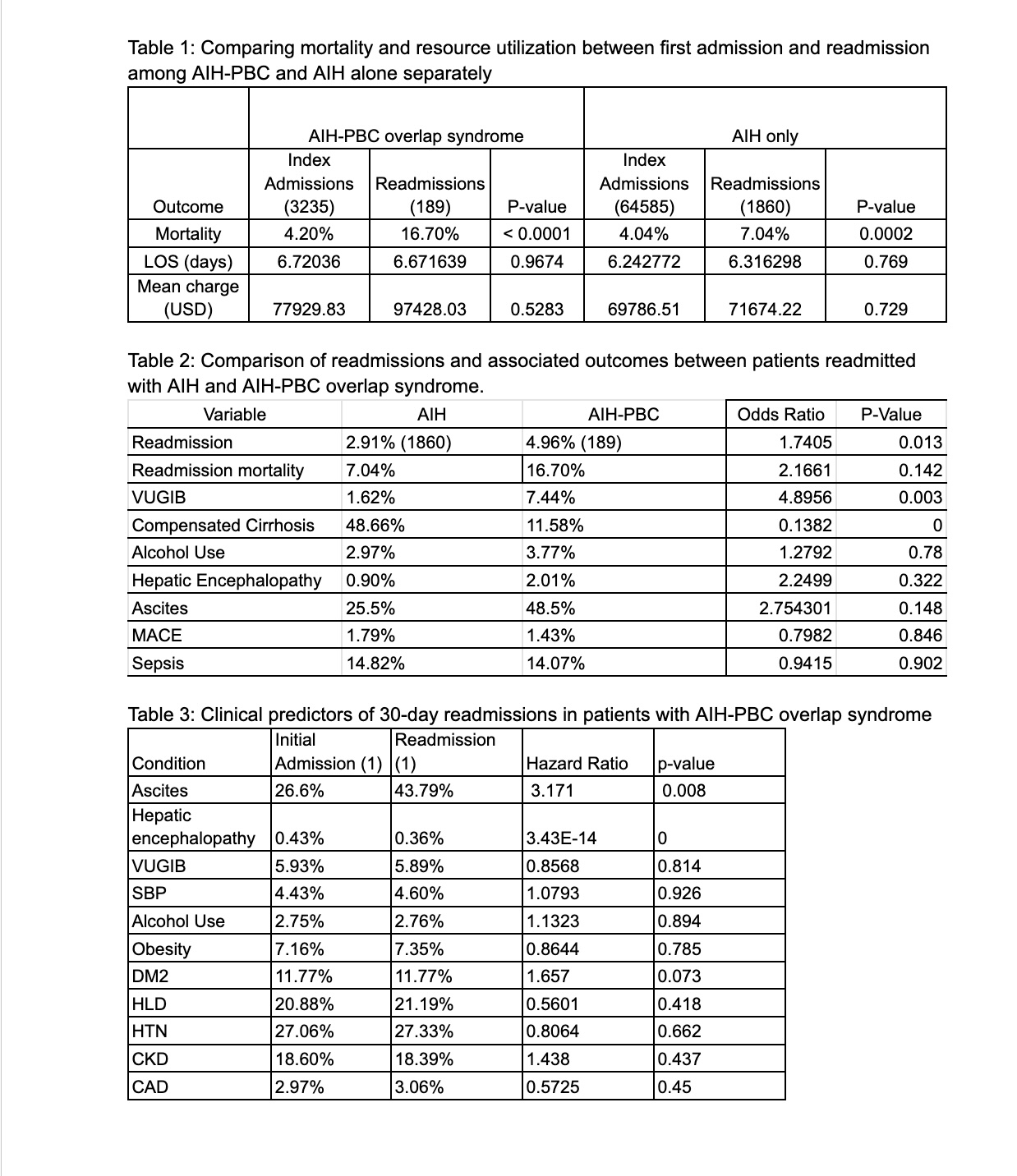
Methods: This study utilized data from the National Readmission Database (2016-2020). Data was analyzed from 32,235 index admissions and 189 readmissions for AIH-PBC overlap syndrome, and 64,585 index admissions and 1,860 readmissions for AIH alone. Key outcomes assessed included mortality, length of stay (LOS), and mean hospital charges. Statistical significance was determined using p-values. Multivariate regression analysis was used to compare the outcomes, presented as odds ratios. Clinical and socio-demographic predictors of 30-day readmissions in AIH-PBC overlap syndrome were studied using Cox regression analysis.
Results: AIH-PBC overlap syndrome had a significantly higher readmission rate (4.96% vs. 2.91%, OR 1.7405, p = 0.013). Patients diagnosed with AIH-PBC overlap syndrome exhibited higher mortality rates during readmission compared to those with AIH alone (16.70% vs. 7.04%, OR = 2.166, p = 0.142). Additionally, AIH-PBC patients showed a significantly higher incidence of variceal upper gastrointestinal bleeding (VUGIB) during readmission compared to AIH alone patients (7.44% vs. 1.62%, OR 4.8956, p = 0.003). Conversely, AIH-PBC patients had a significantly lower incidence of compensated cirrhosis during readmission (11.58% vs. 48.66%, OR 0.1382, p < 0.0001). No significant differences were observed in the rates of ascites, hepatic encephalopathy, alcohol use, major adverse cardiac events (MACE), or sepsis between the two groups.
Discussion: Patients with AIH-PBC overlap syndrome exhibit significantly higher readmission rates and morbidity, and higher mortality upon readmission compared to those with AIH alone. Further research is needed to identify modifiable risk factors and interventions to reduce morbidity, such as closer monitoring of variceal bleed given the higher risk. These findings underscore the need for heightened monitoring and targeted interventions for this high-risk population to improve post-discharge outcomes and healthcare costs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Vinay Jahagirdar, MD3, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB4, Nadeem Anwar, MD5. P1250 - Adverse 30-Day Readmission Outcomes Among Patients Diagnosed with AIH-PBC Overlap Syndrome Compared with AIH Alone, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Indiana University Southwest, Evansville, IN; 5West Virginia University Charleston Area Medical Center, Charleston, WV
Introduction: This study aims to compare 30-day readmission outcomes, mortality rates, and resource utilization between patients diagnosed with Autoimmune Hepatitis-Primary Biliary Cholangitis (AIH-PBC) overlap syndrome and those with Autoimmune Hepatitis (AIH) alone.
Methods: This study utilized data from the National Readmission Database (2016-2020). Data was analyzed from 32,235 index admissions and 189 readmissions for AIH-PBC overlap syndrome, and 64,585 index admissions and 1,860 readmissions for AIH alone. Key outcomes assessed included mortality, length of stay (LOS), and mean hospital charges. Statistical significance was determined using p-values. Multivariate regression analysis was used to compare the outcomes, presented as odds ratios. Clinical and socio-demographic predictors of 30-day readmissions in AIH-PBC overlap syndrome were studied using Cox regression analysis.
Results: AIH-PBC overlap syndrome had a significantly higher readmission rate (4.96% vs. 2.91%, OR 1.7405, p = 0.013). Patients diagnosed with AIH-PBC overlap syndrome exhibited higher mortality rates during readmission compared to those with AIH alone (16.70% vs. 7.04%, OR = 2.166, p = 0.142). Additionally, AIH-PBC patients showed a significantly higher incidence of variceal upper gastrointestinal bleeding (VUGIB) during readmission compared to AIH alone patients (7.44% vs. 1.62%, OR 4.8956, p = 0.003). Conversely, AIH-PBC patients had a significantly lower incidence of compensated cirrhosis during readmission (11.58% vs. 48.66%, OR 0.1382, p < 0.0001). No significant differences were observed in the rates of ascites, hepatic encephalopathy, alcohol use, major adverse cardiac events (MACE), or sepsis between the two groups.
Discussion: Patients with AIH-PBC overlap syndrome exhibit significantly higher readmission rates and morbidity, and higher mortality upon readmission compared to those with AIH alone. Further research is needed to identify modifiable risk factors and interventions to reduce morbidity, such as closer monitoring of variceal bleed given the higher risk. These findings underscore the need for heightened monitoring and targeted interventions for this high-risk population to improve post-discharge outcomes and healthcare costs.
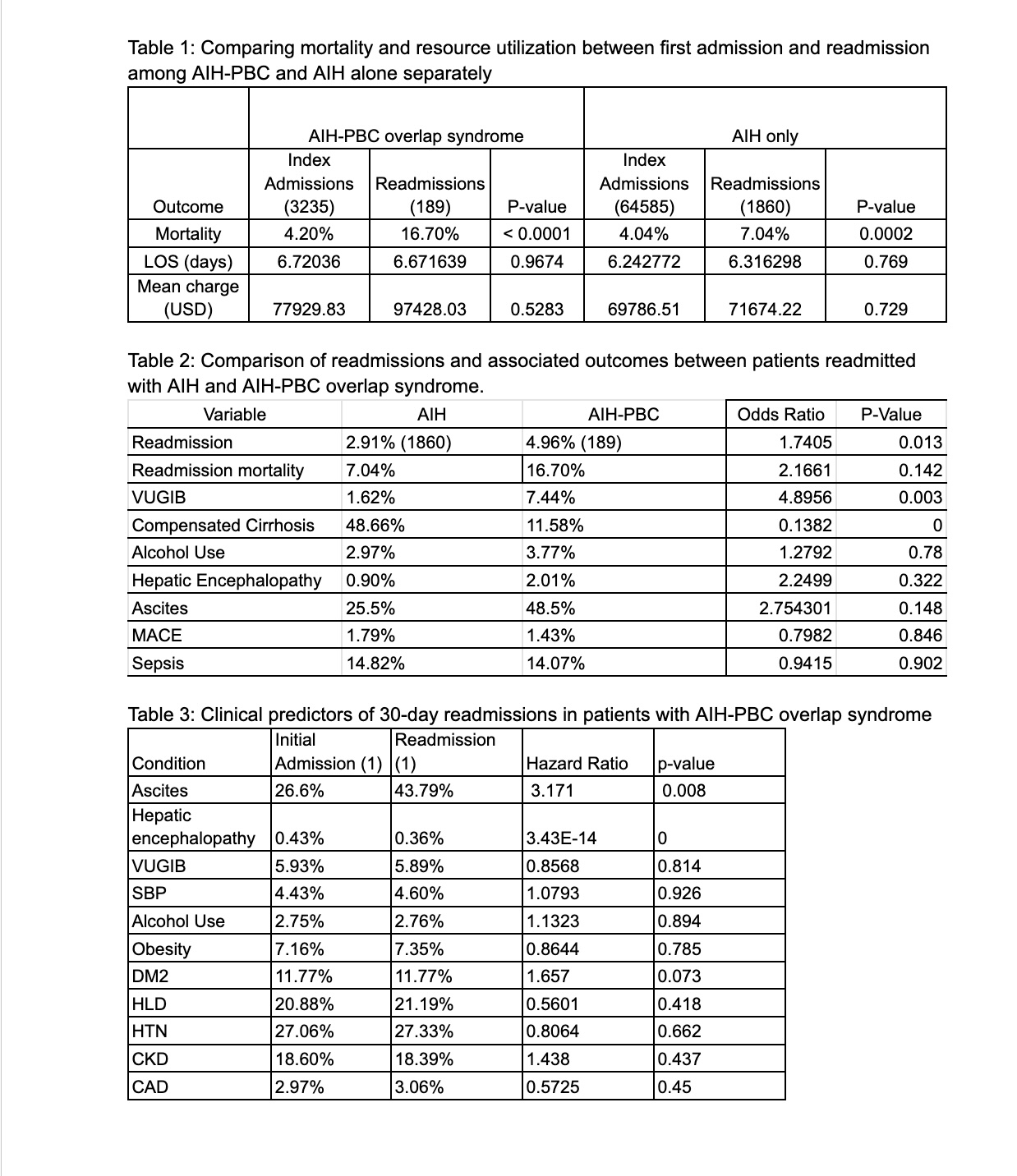
Figure: -Comparing inpatient outcomes, resource utilization between AIH and AIH-PBC syndrome
-Clinical predictors of 30-day readmissions in PBC-AIH overlap syndrome
-Clinical predictors of 30-day readmissions in PBC-AIH overlap syndrome
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Sophia dar indicated no relevant financial relationships.
Muhammad Chaudhary indicated no relevant financial relationships.
Nadeem Anwar indicated no relevant financial relationships.
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Vinay Jahagirdar, MD3, Sophia dar, MD1, Muhammad YN. Chaudhary, MBChB4, Nadeem Anwar, MD5. P1250 - Adverse 30-Day Readmission Outcomes Among Patients Diagnosed with AIH-PBC Overlap Syndrome Compared with AIH Alone, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
