Sunday Poster Session
Category: Liver
P1310 - Navigating Diagnostic Challenges in Hemophagocytic Lymphohistiocytosis: A Complex Clinical Presentation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Dakota Bigham, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Dakota Bigham, MD1, Jonathan Selzman, DO2, James Gnecco, DO2, Fabian Rodas, MD3
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3The Texas Liver Institute, San Antonio, TX
Introduction: Hemophagocytic Lymphohistiocytosis (HLH) represents a rare yet severe hyperinflammatory condition marked by abnormal immune system activation, resulting in extensive tissue injury and organ dysfunction.
Case Description/Methods: Patient is a 72-year-old female with a history of hypertension, recent travel to Thailand, and a recent urinary tract infection (UTI), who presented to an outside hospital with jaundice and dark urine, manifesting approximately 10 days after completing a seven-day course of nitrofurantoin followed by ciprofloxacin due to unresolved symptoms. Apart from Moringa tea and RYZE brand mushrooms, she had no other medication history or high-risk behaviors. Initial suspicion centered on drug-induced liver injury (DILI), supported by biopsy results showing acute cholestatic hepatitis without evidence of chronic liver disease, and notable lack of phagocytic processes. Despite a week-long course of prednisone, symptoms persisted, prompting transfer for further evaluation.
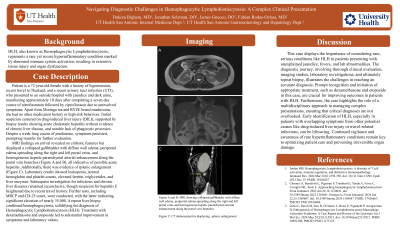
MRI findings on arrival revealed no cirrhotic features but indicated acute hepatitis, alongside splenic enlargement. Lab results showed leukopenia, normal hemoglobin and platelet counts, ferritin over 11,000, elevated triglycerides, and increased aspartate aminotransferase (AST) to 1,300, alanine aminotransferase (ALT) to 2,500, alkaline phosphatase (ALP) to 429, and total bilirubin to 17.8. Investigation for infectious and chronic liver disease, including hepatitis E due to recent travel history, showed negative results, with ferritin peaking over 17,000. MRCP revealed periportal edema and findings consistent with acute hepatitis, and CD-25 count was nearly 35,000. Upon repeat evaluation, the initial liver biopsy was reviewed by a consulting pathologist, confirming hemophagocytosis and solidifying the diagnosis of HLH. Treatment with dexamethasone and etoposide led to improvement in symptoms, with outpatient lab values showing improvement in AST to 79, ALT to 186, ALP to 271, and total bilirubin to 7.0.
Discussion: This case displays the importance of considering rare, serious conditions like HLH in patients presenting with unexplained jaundice, fevers, and severe liver injury. The diagnostic journey, involving thorough clinical evaluation, imaging studies, laboratory investigations, and biopsy, illustrates the challenges in reaching an accurate diagnosis. Prompt recognition and initiation of appropriate treatment are crucial for improving outcomes in patients with HLH.
Disclosures:
Dakota Bigham, MD1, Jonathan Selzman, DO2, James Gnecco, DO2, Fabian Rodas, MD3. P1310 - Navigating Diagnostic Challenges in Hemophagocytic Lymphohistiocytosis: A Complex Clinical Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3The Texas Liver Institute, San Antonio, TX
Introduction: Hemophagocytic Lymphohistiocytosis (HLH) represents a rare yet severe hyperinflammatory condition marked by abnormal immune system activation, resulting in extensive tissue injury and organ dysfunction.
Case Description/Methods: Patient is a 72-year-old female with a history of hypertension, recent travel to Thailand, and a recent urinary tract infection (UTI), who presented to an outside hospital with jaundice and dark urine, manifesting approximately 10 days after completing a seven-day course of nitrofurantoin followed by ciprofloxacin due to unresolved symptoms. Apart from Moringa tea and RYZE brand mushrooms, she had no other medication history or high-risk behaviors. Initial suspicion centered on drug-induced liver injury (DILI), supported by biopsy results showing acute cholestatic hepatitis without evidence of chronic liver disease, and notable lack of phagocytic processes. Despite a week-long course of prednisone, symptoms persisted, prompting transfer for further evaluation.
MRI findings on arrival revealed no cirrhotic features but indicated acute hepatitis, alongside splenic enlargement. Lab results showed leukopenia, normal hemoglobin and platelet counts, ferritin over 11,000, elevated triglycerides, and increased aspartate aminotransferase (AST) to 1,300, alanine aminotransferase (ALT) to 2,500, alkaline phosphatase (ALP) to 429, and total bilirubin to 17.8. Investigation for infectious and chronic liver disease, including hepatitis E due to recent travel history, showed negative results, with ferritin peaking over 17,000. MRCP revealed periportal edema and findings consistent with acute hepatitis, and CD-25 count was nearly 35,000. Upon repeat evaluation, the initial liver biopsy was reviewed by a consulting pathologist, confirming hemophagocytosis and solidifying the diagnosis of HLH. Treatment with dexamethasone and etoposide led to improvement in symptoms, with outpatient lab values showing improvement in AST to 79, ALT to 186, ALP to 271, and total bilirubin to 7.0.
Discussion: This case displays the importance of considering rare, serious conditions like HLH in patients presenting with unexplained jaundice, fevers, and severe liver injury. The diagnostic journey, involving thorough clinical evaluation, imaging studies, laboratory investigations, and biopsy, illustrates the challenges in reaching an accurate diagnosis. Prompt recognition and initiation of appropriate treatment are crucial for improving outcomes in patients with HLH.
Disclosures:
Dakota Bigham indicated no relevant financial relationships.
Jonathan Selzman indicated no relevant financial relationships.
James Gnecco indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Dakota Bigham, MD1, Jonathan Selzman, DO2, James Gnecco, DO2, Fabian Rodas, MD3. P1310 - Navigating Diagnostic Challenges in Hemophagocytic Lymphohistiocytosis: A Complex Clinical Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
