Sunday Poster Session
Category: Liver
P1318 - Stealthy Onset: Unveiling Infiltrative Hepatocellular Carcinoma via Elevated Alkaline Phosphatase
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Shruti Kulkarni, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Shruti Kulkarni, MD1, Charles Cavalaris, MD2, Cesar Taborda, MD3, William Bulkeley, MD4
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3James A. Haley Tampa VA/USF Health, Tampa, FL; 4James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Infiltrative hepatocellular carcinoma (iHCC) is rare, constituting a small fraction of diagnosed HCC cases. Despite screening with labs and imaging, the diagnosis is often made when the disease is at an advanced stage. Herein, we present a case of iHCC made in patient after incidental finding of elevated alkaline phosphatase (ALP) prompted further work up.
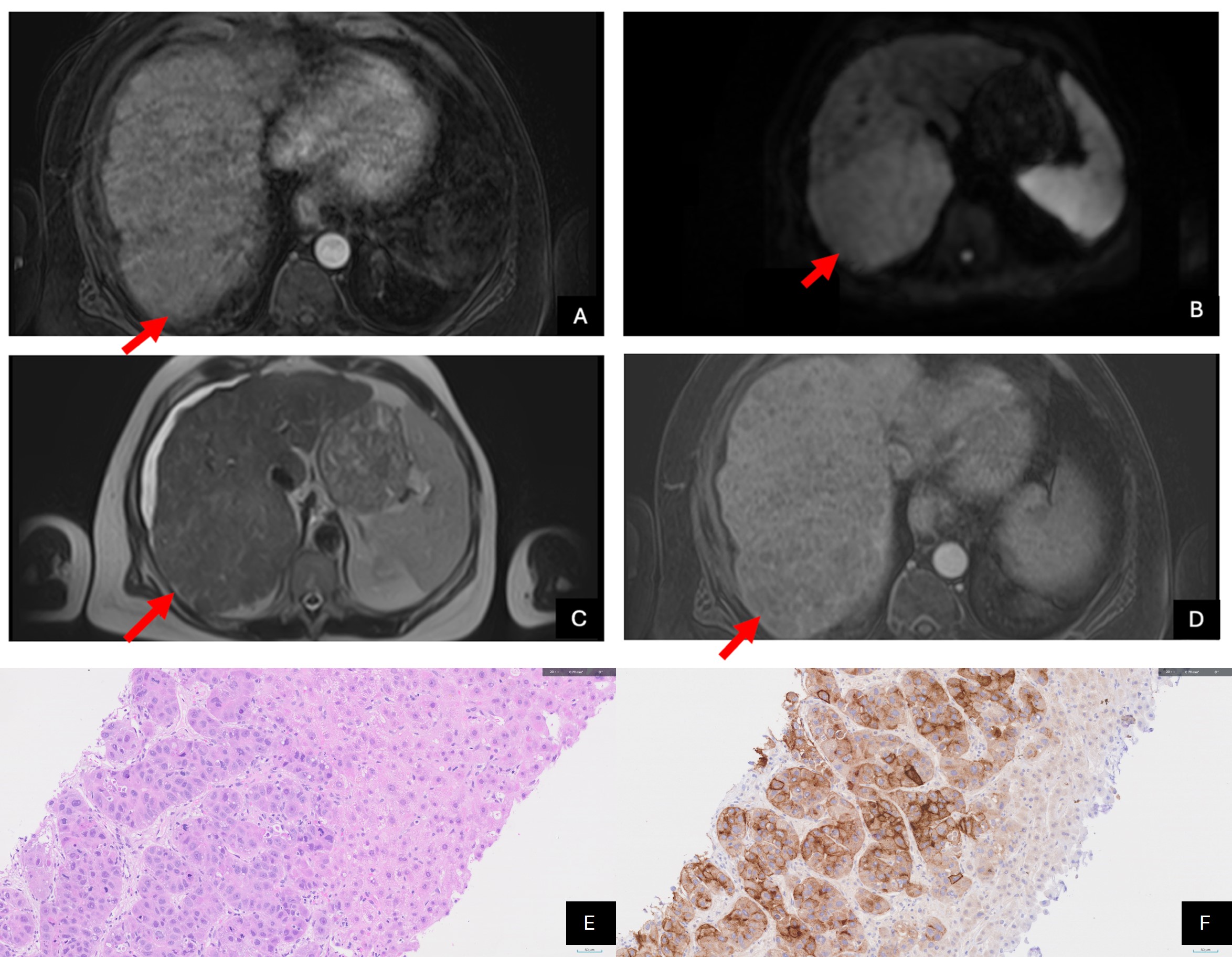
Case Description/Methods: A 61-year-old homeless male veteran with a history of alcoholic cirrhosis presented with symptoms indicative of alcohol withdrawal: abdominal pain, nausea, and vomiting. Initial laboratory tests revealed an AST 45 IU/L, ALT 76 IU/L, and ALP 189 IU/L. Ultrasound and CT imaging did not demonstrate any hepatic lesions. Once symptoms improved, the patient was discharged and advised to follow up outpatient. Two months later, the patient was readmitted for persistent alcohol withdrawal symptoms. ALP levels remained elevated at 324 IU/L. Additional investigation with CT four-phase liver protocol was unremarkable. However, his AFP levels were notably elevated at 1917 ng/mL, compared to 7.0 ng/mL a year prior. Subsequent MRI with contrast revealed a conspicuous area of confluent fibrosis in the right hepatic lobe. Notably, MRI findings (Figure 1A-D) displayed a subtle hyperintense signal on T2 with restricted diffusion on DWI, lack of arterial phase enhancement, and questionable portal venous washout. A targeted liver biopsy confirmed moderately differentiated HCC (Figure 1E-F). Due to the extent of hepatic involvement from aggressive infiltrative nature of the disease and the patient’s quick clinical deterioration, the patient was not a candidate for any therapy. Subsequently, the patient was enrolled in hospice care.
Discussion: The persistently elevated ALP upon readmission raised concerns about hepatobiliary disease, though no significant hepatic lesions were initially detected via imaging. While characteristic imaging findings, such as arterially enhancing hepatic masses, can often indicate HCC, CT imaging was negative and MRI only revealed fibrosis. The diagnostic hurdle lies in distinguishing iHCC from benign confluent fibrosis. Due to the spread of tiny subtle tumor nodules throughout the liver, iHCC is often diagnosed late in the disease course and thus portends a poor prognosis. Notably, this patient case stands out due to the represented population; homeless veterans with cirrhosis face heightened all-cause mortality, likely stemming from significant psychosocial and socioeconomic barriers to adequate healthcare.
Disclosures:
Shruti Kulkarni, MD1, Charles Cavalaris, MD2, Cesar Taborda, MD3, William Bulkeley, MD4. P1318 - Stealthy Onset: Unveiling Infiltrative Hepatocellular Carcinoma via Elevated Alkaline Phosphatase, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3James A. Haley Tampa VA/USF Health, Tampa, FL; 4James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Infiltrative hepatocellular carcinoma (iHCC) is rare, constituting a small fraction of diagnosed HCC cases. Despite screening with labs and imaging, the diagnosis is often made when the disease is at an advanced stage. Herein, we present a case of iHCC made in patient after incidental finding of elevated alkaline phosphatase (ALP) prompted further work up.
Case Description/Methods: A 61-year-old homeless male veteran with a history of alcoholic cirrhosis presented with symptoms indicative of alcohol withdrawal: abdominal pain, nausea, and vomiting. Initial laboratory tests revealed an AST 45 IU/L, ALT 76 IU/L, and ALP 189 IU/L. Ultrasound and CT imaging did not demonstrate any hepatic lesions. Once symptoms improved, the patient was discharged and advised to follow up outpatient. Two months later, the patient was readmitted for persistent alcohol withdrawal symptoms. ALP levels remained elevated at 324 IU/L. Additional investigation with CT four-phase liver protocol was unremarkable. However, his AFP levels were notably elevated at 1917 ng/mL, compared to 7.0 ng/mL a year prior. Subsequent MRI with contrast revealed a conspicuous area of confluent fibrosis in the right hepatic lobe. Notably, MRI findings (Figure 1A-D) displayed a subtle hyperintense signal on T2 with restricted diffusion on DWI, lack of arterial phase enhancement, and questionable portal venous washout. A targeted liver biopsy confirmed moderately differentiated HCC (Figure 1E-F). Due to the extent of hepatic involvement from aggressive infiltrative nature of the disease and the patient’s quick clinical deterioration, the patient was not a candidate for any therapy. Subsequently, the patient was enrolled in hospice care.
Discussion: The persistently elevated ALP upon readmission raised concerns about hepatobiliary disease, though no significant hepatic lesions were initially detected via imaging. While characteristic imaging findings, such as arterially enhancing hepatic masses, can often indicate HCC, CT imaging was negative and MRI only revealed fibrosis. The diagnostic hurdle lies in distinguishing iHCC from benign confluent fibrosis. Due to the spread of tiny subtle tumor nodules throughout the liver, iHCC is often diagnosed late in the disease course and thus portends a poor prognosis. Notably, this patient case stands out due to the represented population; homeless veterans with cirrhosis face heightened all-cause mortality, likely stemming from significant psychosocial and socioeconomic barriers to adequate healthcare.
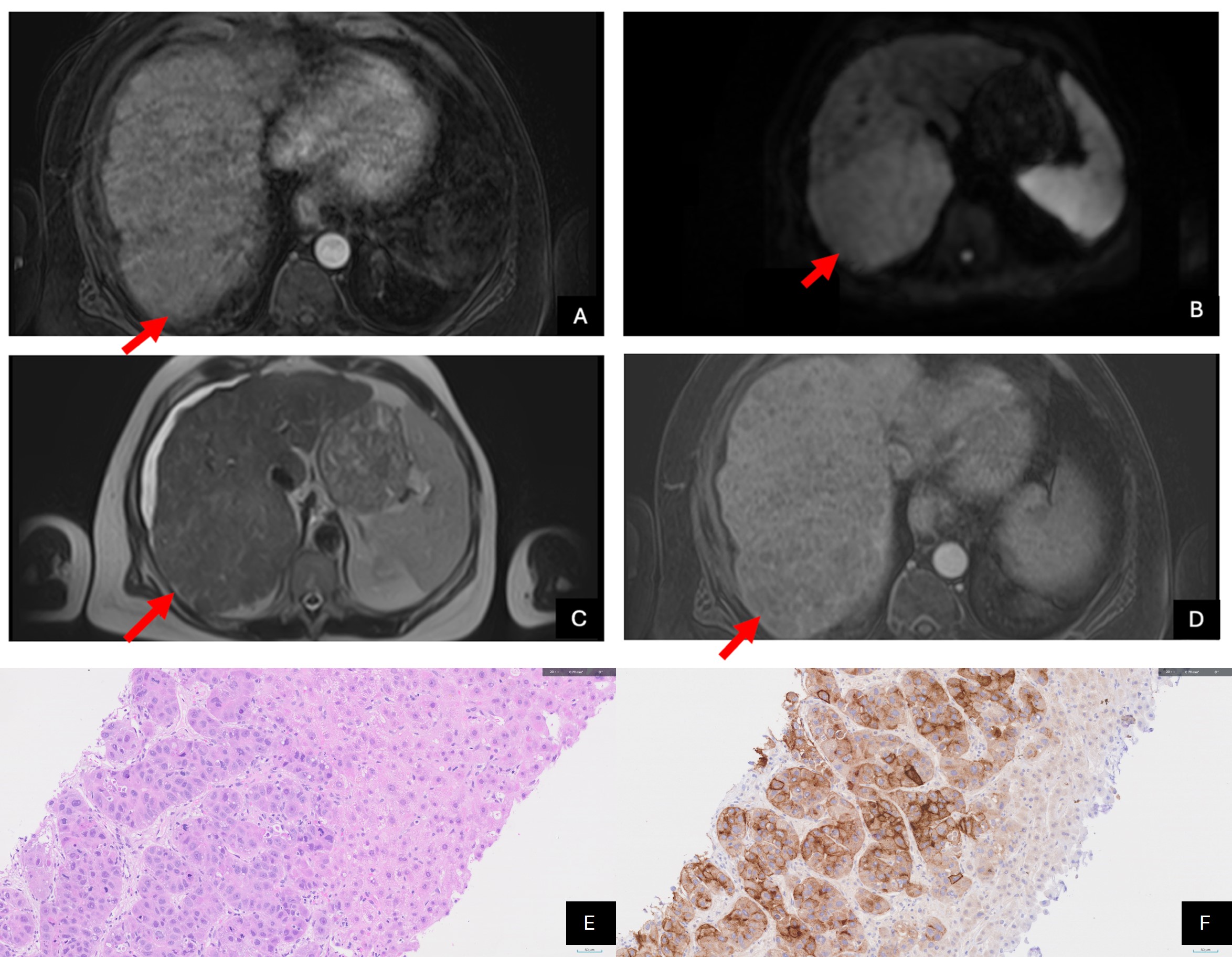
Figure: Figure 1: MRI abdomen with IV contrast demonstrating subtle hyperintense signal on T2 (C), restricted diffusion DWI (B), lack of arterial phase enhancement (D) and questionable portal venous washout (A). Liver biopsy pathology slides showing infiltrative HCC characterized by a trabecular growth pattern alongside adjacent liver parenchyma in top right (E) as well as Glypican immunohistochemical staining showing cytoplasmic positivity in the HCC with differential expression from the background benign hepatocytes (F).
Disclosures:
Shruti Kulkarni indicated no relevant financial relationships.
Charles Cavalaris indicated no relevant financial relationships.
Cesar Taborda indicated no relevant financial relationships.
William Bulkeley indicated no relevant financial relationships.
Shruti Kulkarni, MD1, Charles Cavalaris, MD2, Cesar Taborda, MD3, William Bulkeley, MD4. P1318 - Stealthy Onset: Unveiling Infiltrative Hepatocellular Carcinoma via Elevated Alkaline Phosphatase, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
