Sunday Poster Session
Category: Liver
P1328 - Type 2 Idiopathic Adult Ductopenia in a Male with Decompensated Biliary Cirrhosis - An Etiological Conundrum
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kojo-Frimpong B. Awuah, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Kojo-Frimpong B. Awuah, MD, Ravi Ranganatha, MD, Tyrell Daniel, MD, Kingsley Ozongwu, MD, Alexandra M. Johnston, DO
Allegheny General Hospital, Pittsburgh, PA
Introduction: Idiopathic adulthood ductopenia (IAD) is a rare condition characterized by the destruction and disappearance of intrahepatic bile ducts. The etiology is typically unknown, however immune, infectious, and malignant processes may be associated. We present a rare case of IAD in a patient with no identifiable risk factors who eventually required a liver transplant.
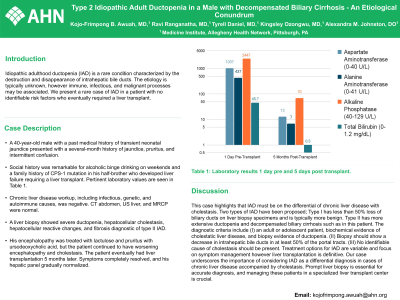
Case Description/Methods: A 40-year-old male with a past medical history of transient neonatal jaundice came in with a several-month history of jaundice, pruritus, and intermittent confusion. Social history was remarkable for alcoholic binge drinking on weekends and a family history of CPS-1 mutation in his half-brother who developed liver failure requiring a liver transplant. Pertinent laboratory values are seen in Table 1. Chronic liver disease workup including infectious, genetic and autoimmune causes were negative. CT abdomen, US liver, and MRCP were normal. A liver biopsy showed severe ductopenia, hepatocellular cholestasis, hepatocellular reactive changes, and fibrosis diagnostic of type II IAD. His encephalopathy was treated with lactulose and pruritus with ursodeoxycholic acid, but the patient continued to have worsening encephalopathy and cholestasis. The patient eventually had liver transplantation 5 months later. Symptoms completely resolved and his hepatic panel gradually normalized.
Discussion: This case highlights that IAD must be on the differential of chronic liver disease with cholestasis. Two types of IAD have been proposed; Type I has less than 50% loss of biliary ducts on liver biopsy specimens and is typically more benign. Type II has more extensive ductopenia and decompensated biliary cirrhosis such as in this patient. The diagnostic criteria include (I) an adult or adolescent patient, biochemical evidence of cholestatic liver disease, and biopsy evidence of ductopenia. (II) Biopsy should show a decrease in intrahepatic bile ducts in at least 50% of the portal tracts. (III) No identifiable cause of cholestasis should be present. Treatment options for IAD are variable and focus on symptom management however liver transplantation is definitive. Our case underscores the importance of considering IAD as a differential diagnosis in cases of chronic liver disease accompanied by cholestasis. Prompt liver biopsy is essential for accurate diagnosis, and managing these patients in a specialized liver transplant center is crucial.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kojo-Frimpong B. Awuah, MD, Ravi Ranganatha, MD, Tyrell Daniel, MD, Kingsley Ozongwu, MD, Alexandra M. Johnston, DO. P1328 - Type 2 Idiopathic Adult Ductopenia in a Male with Decompensated Biliary Cirrhosis - An Etiological Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Allegheny General Hospital, Pittsburgh, PA
Introduction: Idiopathic adulthood ductopenia (IAD) is a rare condition characterized by the destruction and disappearance of intrahepatic bile ducts. The etiology is typically unknown, however immune, infectious, and malignant processes may be associated. We present a rare case of IAD in a patient with no identifiable risk factors who eventually required a liver transplant.
Case Description/Methods: A 40-year-old male with a past medical history of transient neonatal jaundice came in with a several-month history of jaundice, pruritus, and intermittent confusion. Social history was remarkable for alcoholic binge drinking on weekends and a family history of CPS-1 mutation in his half-brother who developed liver failure requiring a liver transplant. Pertinent laboratory values are seen in Table 1. Chronic liver disease workup including infectious, genetic and autoimmune causes were negative. CT abdomen, US liver, and MRCP were normal. A liver biopsy showed severe ductopenia, hepatocellular cholestasis, hepatocellular reactive changes, and fibrosis diagnostic of type II IAD. His encephalopathy was treated with lactulose and pruritus with ursodeoxycholic acid, but the patient continued to have worsening encephalopathy and cholestasis. The patient eventually had liver transplantation 5 months later. Symptoms completely resolved and his hepatic panel gradually normalized.
Discussion: This case highlights that IAD must be on the differential of chronic liver disease with cholestasis. Two types of IAD have been proposed; Type I has less than 50% loss of biliary ducts on liver biopsy specimens and is typically more benign. Type II has more extensive ductopenia and decompensated biliary cirrhosis such as in this patient. The diagnostic criteria include (I) an adult or adolescent patient, biochemical evidence of cholestatic liver disease, and biopsy evidence of ductopenia. (II) Biopsy should show a decrease in intrahepatic bile ducts in at least 50% of the portal tracts. (III) No identifiable cause of cholestasis should be present. Treatment options for IAD are variable and focus on symptom management however liver transplantation is definitive. Our case underscores the importance of considering IAD as a differential diagnosis in cases of chronic liver disease accompanied by cholestasis. Prompt liver biopsy is essential for accurate diagnosis, and managing these patients in a specialized liver transplant center is crucial.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kojo-Frimpong Awuah indicated no relevant financial relationships.
Ravi Ranganatha indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Kingsley Ozongwu indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah, MD, Ravi Ranganatha, MD, Tyrell Daniel, MD, Kingsley Ozongwu, MD, Alexandra M. Johnston, DO. P1328 - Type 2 Idiopathic Adult Ductopenia in a Male with Decompensated Biliary Cirrhosis - An Etiological Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
