Sunday Poster Session
Category: Liver
P1329 - SARS-CoV-2 Induced Variceal Bleeding in Patient With Chronic Portal Vein Thrombosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kojo-Frimpong B. Awuah, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Tyrell Daniel, MD1, Kojo-Frimpong B. Awuah, MD1, Kingsley Ozongwu, MD1, Matthew D. Simpson, MD1, Edmund Appiah-Kubi, MD1, Alexandra M. Johnston, DO2
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA
Introduction: Portal vein thrombosis (PVT) is a rare etiology of non-cirrhotic portal hypertension (PH) with an incidence of 1-2%. Variceal bleeding secondary to chronic PVT may occur at a rate of 4.5-8%. Here we present a case of initial variceal bleeding induced by SARS-CoV-2 in a patient with a 3-year history of chronic PVT.
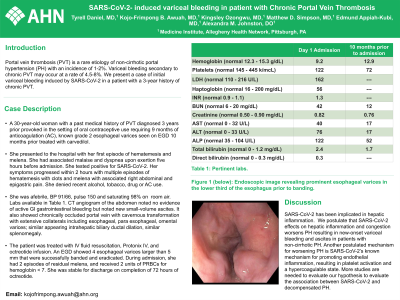
Case Description/Methods: The patient is a 30-year-old woman with a past medical history of PVT diagnosed 3 years prior provoked in the setting of oral contraceptive use requiring 9 months of anticoagulation (AC), known grade 2 esophageal varices seen on EGD 10 months prior treated with carvedilol. She presented to the hospital with her first episode of hematemesis and melena. She had associated malaise and dyspnea upon exertion five hours before admission. She tested positive for SARS-CoV-2. Her symptoms progressed within 2 hours with multiple episodes of hematemesis with clots and melena with associated right abdominal and epigastric pain. She denied recent alcohol, tobacco, drug or AC use. She was afebrile, BP 91/66, pulse 150 and saturating 98% on room air. Labs seen in Table 1. CT angiogram of the abdomen noted no evidence of active GI gastrointestinal bleeding but noted new small-volume ascites. It also showed chronically occluded portal vein with cavernous transformation with extensive collaterals including esophageal, para esophageal, omental varices; similar appearing intrahepatic biliary ductal dilation, similar splenomegaly. The patient was treated with IV fluid resuscitation, Protonix IV, and octreotide infusion. An EGD showed 4 esophageal varices larger than 5 mm that were successfully banded and eradicated. During admission, she had 2 episodes of residual melena, and received 2 units of PRBCs for hemoglobin < 7. She was stable for discharge on completion of 72 hours of octreotide.
Discussion: SARS-CoV-2 has been implicated in hepatic inflammation. We postulate that SARS-CoV-2 effects on hepatic inflammation and congestion worsens PH resulting in new-onset variceal bleeding and ascites in patients with non-cirrhotic PH. Another postulated mechanism for worsening PH is SARS-CoV-2’s known mechanism for promoting endothelial inflammation, resulting in platelet activation and a hypercoagulable state. More studies are needed to evaluate our hypothesis to evaluate the association between SARS-CoV-2 and decompensated PH.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tyrell Daniel, MD1, Kojo-Frimpong B. Awuah, MD1, Kingsley Ozongwu, MD1, Matthew D. Simpson, MD1, Edmund Appiah-Kubi, MD1, Alexandra M. Johnston, DO2. P1329 - SARS-CoV-2 Induced Variceal Bleeding in Patient With Chronic Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA
Introduction: Portal vein thrombosis (PVT) is a rare etiology of non-cirrhotic portal hypertension (PH) with an incidence of 1-2%. Variceal bleeding secondary to chronic PVT may occur at a rate of 4.5-8%. Here we present a case of initial variceal bleeding induced by SARS-CoV-2 in a patient with a 3-year history of chronic PVT.
Case Description/Methods: The patient is a 30-year-old woman with a past medical history of PVT diagnosed 3 years prior provoked in the setting of oral contraceptive use requiring 9 months of anticoagulation (AC), known grade 2 esophageal varices seen on EGD 10 months prior treated with carvedilol. She presented to the hospital with her first episode of hematemesis and melena. She had associated malaise and dyspnea upon exertion five hours before admission. She tested positive for SARS-CoV-2. Her symptoms progressed within 2 hours with multiple episodes of hematemesis with clots and melena with associated right abdominal and epigastric pain. She denied recent alcohol, tobacco, drug or AC use. She was afebrile, BP 91/66, pulse 150 and saturating 98% on room air. Labs seen in Table 1. CT angiogram of the abdomen noted no evidence of active GI gastrointestinal bleeding but noted new small-volume ascites. It also showed chronically occluded portal vein with cavernous transformation with extensive collaterals including esophageal, para esophageal, omental varices; similar appearing intrahepatic biliary ductal dilation, similar splenomegaly. The patient was treated with IV fluid resuscitation, Protonix IV, and octreotide infusion. An EGD showed 4 esophageal varices larger than 5 mm that were successfully banded and eradicated. During admission, she had 2 episodes of residual melena, and received 2 units of PRBCs for hemoglobin < 7. She was stable for discharge on completion of 72 hours of octreotide.
Discussion: SARS-CoV-2 has been implicated in hepatic inflammation. We postulate that SARS-CoV-2 effects on hepatic inflammation and congestion worsens PH resulting in new-onset variceal bleeding and ascites in patients with non-cirrhotic PH. Another postulated mechanism for worsening PH is SARS-CoV-2’s known mechanism for promoting endothelial inflammation, resulting in platelet activation and a hypercoagulable state. More studies are needed to evaluate our hypothesis to evaluate the association between SARS-CoV-2 and decompensated PH.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tyrell Daniel indicated no relevant financial relationships.
Kojo-Frimpong Awuah indicated no relevant financial relationships.
Kingsley Ozongwu indicated no relevant financial relationships.
Matthew Simpson indicated no relevant financial relationships.
Edmund Appiah-Kubi indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Tyrell Daniel, MD1, Kojo-Frimpong B. Awuah, MD1, Kingsley Ozongwu, MD1, Matthew D. Simpson, MD1, Edmund Appiah-Kubi, MD1, Alexandra M. Johnston, DO2. P1329 - SARS-CoV-2 Induced Variceal Bleeding in Patient With Chronic Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
