Sunday Poster Session
Category: Liver
P1335 - Iatrogenic Mucosal Kaposi’s Sarcoma in a Heart-Liver Transplant Recipient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hannah O'Neill, MD
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Hannah O'Neill, MD1, Shayan Amini, MD2, Apaar Dadlani, MBBS1, Michelle Jones-Pauley, DO1, Tamneet Basra, MD1, David W. Victor, MD1, Sudha Kodali, MD, MSPH1
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX
Introduction: Kaposi’s Sarcoma (KS) is an angioproliferative malignancy typically characterized by cutaneous lesions induced by human Herpesviridae 8 (HHV-8). Iatrogenic KS is a well-known complication of immunosuppression and often associated with an anti-rejection regimen following solid organ transplant. Following diagnosis, management requires immunosuppressive adjustment for KS treatment.
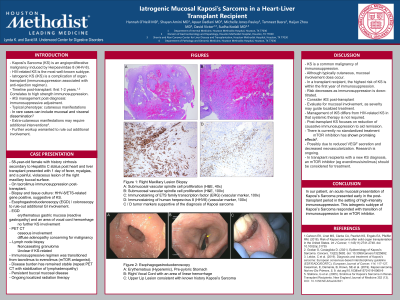
Case Description/Methods: A 58 yr-old female with past medical history of cirrhosis secondary to Hepatitis C and diastolic heart failure, status post heart and liver transplant on tacrolimus immunosuppression presented with 1 day of fever, myalgias, and a painful, violaceous lesion of the right maxillary buccal surface. Biopsy and tissue culture were HHV-8/ETS-related gene positive, suggestive of KS. In setting of mucosal presentation of KS, patient underwent esophogastroduodenoscopy (EGD) /colonoscopy to rule-out additional GI involvement. EGD found erythematous gastric mucosa (reactive gastropathy) and an area of vocal cord hemorrhage and ruled out further KS involvement. PET CT found osseous involvement and diffuse adenopathy concerning for malignancy – subsequent LN biopsy showed noncaseating granuloma that was not KS (nondiagnostic). Patient’s immunosuppressive regimen was transitioned from tacrolimus to everolimus (mTOR antagonist) and patient follows with oncology for disease course monitoring.
Discussion: KS is a common malignancy of immunosuppression. Although typically cutaneous, mucosal involvement does occur. In a transplant recipient, the highest risk of KS is within the first year of immunosuppression, and risk decreases as immunosuppression is down-titrated. KS should be considered and further evaluated in any transplant recipient with cutaneous/mucosal changes, and particularly early post-transplant. In patients with mucosal involvement, further GI evaluation to determine the extent of mucosal involvement should be considered; severity may guide localized treatment.
Management of Iatrogenic KS differs from Classic KS in that systemic therapy is not required. Management focuses on reduction of causative immunosuppression to aid remission. There is currently no standardized treatment, however, mTOR inhibition has shown early promising effects. This may be due to reduced VEGF secretion and thus decreased neovascularization, although research is ongoing. In transplant recipients with a new KS diagnosis, an mTOR inhibitor (eg everolimus/sirolimus) should be considered for treatment.
Disclosures:
Hannah O'Neill, MD1, Shayan Amini, MD2, Apaar Dadlani, MBBS1, Michelle Jones-Pauley, DO1, Tamneet Basra, MD1, David W. Victor, MD1, Sudha Kodali, MD, MSPH1. P1335 - Iatrogenic Mucosal Kaposi’s Sarcoma in a Heart-Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX
Introduction: Kaposi’s Sarcoma (KS) is an angioproliferative malignancy typically characterized by cutaneous lesions induced by human Herpesviridae 8 (HHV-8). Iatrogenic KS is a well-known complication of immunosuppression and often associated with an anti-rejection regimen following solid organ transplant. Following diagnosis, management requires immunosuppressive adjustment for KS treatment.
Case Description/Methods: A 58 yr-old female with past medical history of cirrhosis secondary to Hepatitis C and diastolic heart failure, status post heart and liver transplant on tacrolimus immunosuppression presented with 1 day of fever, myalgias, and a painful, violaceous lesion of the right maxillary buccal surface. Biopsy and tissue culture were HHV-8/ETS-related gene positive, suggestive of KS. In setting of mucosal presentation of KS, patient underwent esophogastroduodenoscopy (EGD) /colonoscopy to rule-out additional GI involvement. EGD found erythematous gastric mucosa (reactive gastropathy) and an area of vocal cord hemorrhage and ruled out further KS involvement. PET CT found osseous involvement and diffuse adenopathy concerning for malignancy – subsequent LN biopsy showed noncaseating granuloma that was not KS (nondiagnostic). Patient’s immunosuppressive regimen was transitioned from tacrolimus to everolimus (mTOR antagonist) and patient follows with oncology for disease course monitoring.
Discussion: KS is a common malignancy of immunosuppression. Although typically cutaneous, mucosal involvement does occur. In a transplant recipient, the highest risk of KS is within the first year of immunosuppression, and risk decreases as immunosuppression is down-titrated. KS should be considered and further evaluated in any transplant recipient with cutaneous/mucosal changes, and particularly early post-transplant. In patients with mucosal involvement, further GI evaluation to determine the extent of mucosal involvement should be considered; severity may guide localized treatment.
Management of Iatrogenic KS differs from Classic KS in that systemic therapy is not required. Management focuses on reduction of causative immunosuppression to aid remission. There is currently no standardized treatment, however, mTOR inhibition has shown early promising effects. This may be due to reduced VEGF secretion and thus decreased neovascularization, although research is ongoing. In transplant recipients with a new KS diagnosis, an mTOR inhibitor (eg everolimus/sirolimus) should be considered for treatment.
Disclosures:
Hannah O'Neill indicated no relevant financial relationships.
Shayan Amini indicated no relevant financial relationships.
Apaar Dadlani indicated no relevant financial relationships.
Michelle Jones-Pauley indicated no relevant financial relationships.
Tamneet Basra indicated no relevant financial relationships.
David Victor: Gilead – speaker fees. Intercept Pharmaceuticals, Inc. – Advisory Committee/Board Member, Consultant, Speaker fees. Sebela – Consultant.
Sudha Kodali: ASTRAZENECA – Advisory Committee/Board Member. GILEAD – Speakers Bureau. SIRTEX – Advisory Committee/Board Member.
Hannah O'Neill, MD1, Shayan Amini, MD2, Apaar Dadlani, MBBS1, Michelle Jones-Pauley, DO1, Tamneet Basra, MD1, David W. Victor, MD1, Sudha Kodali, MD, MSPH1. P1335 - Iatrogenic Mucosal Kaposi’s Sarcoma in a Heart-Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
