Sunday Poster Session
Category: Liver
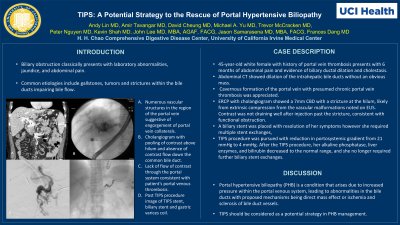
P1343 - TIPS: A Potential Strategy to the Rescue of Portal Hypertensive Biliopathy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AL
Andy L. Lin, MD
University of California, Irvine
Orange, CA
Presenting Author(s)
Andy L. Lin, MD1, Amirali Tavangar, MD1, David L. Cheung, MD1, Michael Andrew Yu, MD1, Trevor McCracken, MD2, Peter H. Nguyen, MD1, Jason Samarasena, MD1, John G. Lee, MD1, Kevin P. Shah, MD3, Frances Dang, MD1
1University of California, Irvine, Orange, CA; 2University of California Irvine, Orange, CA; 3Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Biliary obstruction classically presents with laboratory abnormalities, jaundice, and abdominal pain. Common etiologies include gallstones, tumors and strictures within the bile ducts impairing bile flow. We present a case of portal vein thrombosis with cavernous transformation as an unusual cause of biliary obstruction.
Case Description/Methods: A 45-year-old white female with history of portal vein thrombosis presented to our medical center for evaluation of 6 months of abdominal pain with biliary ductal dilation and cholestasis. Abdominal CT showed dilation of the intrahepatic bile ducts without an obvious mass. Cavernous formation of the portal vein with presumed chronic portal vein thrombosis was appreciated. An MRCP revealed intrahepatic biliary dilatation to the level of bifurcation, however proximal CBD was not well visualized due to flow artifact from adjacent cavernous transformation of the portal vein. No convincing mass lesion was seen. We performed EUS which showed multiple dilated collaterals around the liver hilum appearing to compress the CBD. There was no solid mass to account for the dilation. ERCP with cholangiogram showed a 7mm CBD with a stricture at the hilum, likely from extrinsic compression from the vascular malformations noted on EUS. Contrast was not draining well after injection past the stricture, consistent with functional obstruction. A biliary stent was placed with resolution of her symptoms. She required repeat ERCP with stent exchanges, and eventually underwent TIPS procedure with reduction in portosystemic gradient from 21 mmHg to 4 mmHg. After the TIPS procedure, her alkaline phosphatase, liver enzymes, and bilirubin decreased to the normal range, and she no longer required further biliary stent exchanges.
Discussion: Portal hypertensive biliopathy (PHB) is a condition that arises due to increased pressure within the portal venous system, leading to abnormalities in the bile ducts with proposed mechanisms being direct mass effect or ischemia and sclerosis of bile duct vessels. As TIPS resolved our patient’s biochemical abnormalities and symptoms, our case likely represents the former. As for biliary obstruction in PHB, stent placement may temporarily relieve obstruction; however, stents may have complications and require routine exchange. TIPS should be considered as a strategy in PHB.
Disclosures:
Andy L. Lin, MD1, Amirali Tavangar, MD1, David L. Cheung, MD1, Michael Andrew Yu, MD1, Trevor McCracken, MD2, Peter H. Nguyen, MD1, Jason Samarasena, MD1, John G. Lee, MD1, Kevin P. Shah, MD3, Frances Dang, MD1. P1343 - TIPS: A Potential Strategy to the Rescue of Portal Hypertensive Biliopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California, Irvine, Orange, CA; 2University of California Irvine, Orange, CA; 3Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Biliary obstruction classically presents with laboratory abnormalities, jaundice, and abdominal pain. Common etiologies include gallstones, tumors and strictures within the bile ducts impairing bile flow. We present a case of portal vein thrombosis with cavernous transformation as an unusual cause of biliary obstruction.
Case Description/Methods: A 45-year-old white female with history of portal vein thrombosis presented to our medical center for evaluation of 6 months of abdominal pain with biliary ductal dilation and cholestasis. Abdominal CT showed dilation of the intrahepatic bile ducts without an obvious mass. Cavernous formation of the portal vein with presumed chronic portal vein thrombosis was appreciated. An MRCP revealed intrahepatic biliary dilatation to the level of bifurcation, however proximal CBD was not well visualized due to flow artifact from adjacent cavernous transformation of the portal vein. No convincing mass lesion was seen. We performed EUS which showed multiple dilated collaterals around the liver hilum appearing to compress the CBD. There was no solid mass to account for the dilation. ERCP with cholangiogram showed a 7mm CBD with a stricture at the hilum, likely from extrinsic compression from the vascular malformations noted on EUS. Contrast was not draining well after injection past the stricture, consistent with functional obstruction. A biliary stent was placed with resolution of her symptoms. She required repeat ERCP with stent exchanges, and eventually underwent TIPS procedure with reduction in portosystemic gradient from 21 mmHg to 4 mmHg. After the TIPS procedure, her alkaline phosphatase, liver enzymes, and bilirubin decreased to the normal range, and she no longer required further biliary stent exchanges.
Discussion: Portal hypertensive biliopathy (PHB) is a condition that arises due to increased pressure within the portal venous system, leading to abnormalities in the bile ducts with proposed mechanisms being direct mass effect or ischemia and sclerosis of bile duct vessels. As TIPS resolved our patient’s biochemical abnormalities and symptoms, our case likely represents the former. As for biliary obstruction in PHB, stent placement may temporarily relieve obstruction; however, stents may have complications and require routine exchange. TIPS should be considered as a strategy in PHB.
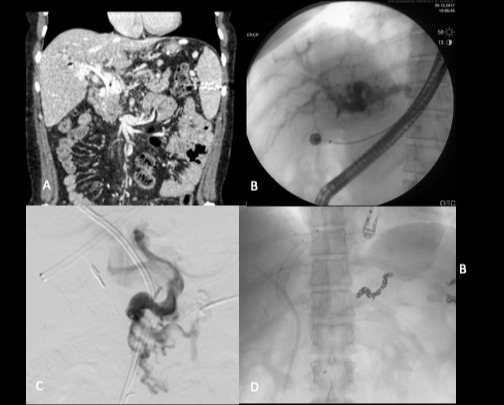
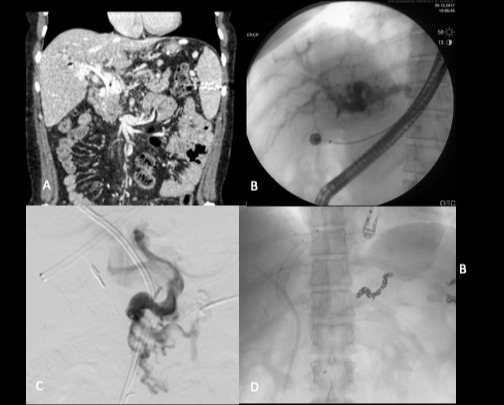
Figure: A. Numerous vascular structures in the region of the portal vein.
B. Cholangiogram with pooling of contrast above hilum and absence of contrast flow down the common bile duct.
C. Absence of flow of contrast through the portal system consistent with patient's portal venous thrombosis
D. Post TIPS procedure image of TIPS stent, biliary stent and gastric varices coils.
B. Cholangiogram with pooling of contrast above hilum and absence of contrast flow down the common bile duct.
C. Absence of flow of contrast through the portal system consistent with patient's portal venous thrombosis
D. Post TIPS procedure image of TIPS stent, biliary stent and gastric varices coils.
Disclosures:
Andy Lin indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
David Cheung indicated no relevant financial relationships.
Michael Andrew Yu indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Jason Samarasena: Cook Medical – Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Neptune Medical – Advisory Committee/Board Member, Consultant. Olympus – Advisory Committee/Board Member, Consultant. Ovesco – Advisory Committee/Board Member, Consultant, Speakers Bureau. SatisfAI – Stock-privately held company. Steris – Advisory Committee/Board Member.
John Lee indicated no relevant financial relationships.
Kevin Shah indicated no relevant financial relationships.
Frances Dang indicated no relevant financial relationships.
Andy L. Lin, MD1, Amirali Tavangar, MD1, David L. Cheung, MD1, Michael Andrew Yu, MD1, Trevor McCracken, MD2, Peter H. Nguyen, MD1, Jason Samarasena, MD1, John G. Lee, MD1, Kevin P. Shah, MD3, Frances Dang, MD1. P1343 - TIPS: A Potential Strategy to the Rescue of Portal Hypertensive Biliopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
