Sunday Poster Session
Category: Liver
P1376 - A Rare Case of Spontaneous Bacterial Peritonitis in a Patient With Heart Failure and Alcohol-Associated Liver Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Jose Garcia-Corella, MD
Kern Medical Center
Bakersfield, CA
Presenting Author(s)
Jose Garcia-Corella, MD, Mahum Zahid, MD, Kevin Dao, MD, Leila Moosavi, MD, Ishaan Kalha, MD
Kern Medical Center, Bakersfield, CA
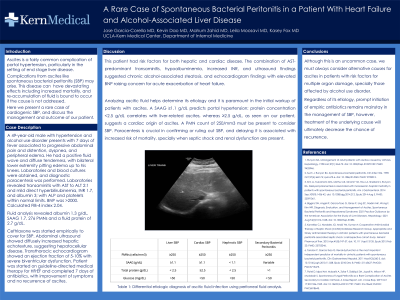
Introduction: Ascites is a fairly common complication of portal hypertension, particularly from liver cirrhosis. Complications from ascites like spontaneous bacterial peritonitis (SBP) may arise. This disease can have devastating effects including increased mortality, and reaccumulation of fluid is bound to occur if the cause is not addressed. Here we would like to present a rare case of cardiogenic SBP and discuss the management and outcome of our patient.
Case Description/Methods: A 49 year-old male with hypertension and alcohol use disorder presents with 7 days of progressive abdominal pain and distention, fever, dyspnea and peripheral edema. He had a positive fluid wave and diffuse tenderness, with bilateral lower extremity pitting edema up to his knees. Laboratories and blood cultures were obtained, and diagnostic paracentesis was performed. Fluid analysis revealed albumin 1.3 g/dL, SAAG 1.7, 276 PMNs and fluid protein 2.7 g/dL. The rest of laboratories showed transaminitis with AST predominance, elevated BNP, and lymphopenia, normal ALP, platelets and TP/TTP.
Ceftriaxone 2 gr daily was empirically started. Abdominal ultrasound showed increased hepatic echotexture suggesting hepatocellular disease. Transthoracic echocardiogram showed an EF of 5% with severe biventricular dysfunction. Appropriate therapy for heart failure with reduced ejection fraction was started and the patient completed 7 days of antibiotic, showing significant improvement of symptoms without recurrence of ascites.
Discussion: This patient had risk factors for both hepatic and cardiac disease, with transaminases and ultrasound findings suggesting chronic liver damage, but BNP and echocardiogram suggesting acute exacerbated heart failure. Analyzing ascitic fluid helps determine its etiology. A SAAG ≥ 1.1 g/dL predicts portal hypertension; protein concentration < 2.5 g/dL correlates with liver-related ascites, whereas ≥ 2.5 g/dL, as seen on our patient, suggests a cardiac origin of ascites. A PMN count of ≥ 250/mm3 must be present to consider SBP.
Paracentesis is crucial in confirming or ruling out SBP, and delaying it is associated with increased mortality. Although this is an uncommon case, when presented with a patient with risk factors for multiple organ damage, one must always consider alternate causes and contributing factors for their symptoms. Regardless of its etiology, prompt initiation of empiric treatment remains mainstay in the treatment of SBP, however, treating the underlying cause decreases the chance of recurrence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jose Garcia-Corella, MD, Mahum Zahid, MD, Kevin Dao, MD, Leila Moosavi, MD, Ishaan Kalha, MD. P1376 - A Rare Case of Spontaneous Bacterial Peritonitis in a Patient With Heart Failure and Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kern Medical Center, Bakersfield, CA
Introduction: Ascites is a fairly common complication of portal hypertension, particularly from liver cirrhosis. Complications from ascites like spontaneous bacterial peritonitis (SBP) may arise. This disease can have devastating effects including increased mortality, and reaccumulation of fluid is bound to occur if the cause is not addressed. Here we would like to present a rare case of cardiogenic SBP and discuss the management and outcome of our patient.
Case Description/Methods: A 49 year-old male with hypertension and alcohol use disorder presents with 7 days of progressive abdominal pain and distention, fever, dyspnea and peripheral edema. He had a positive fluid wave and diffuse tenderness, with bilateral lower extremity pitting edema up to his knees. Laboratories and blood cultures were obtained, and diagnostic paracentesis was performed. Fluid analysis revealed albumin 1.3 g/dL, SAAG 1.7, 276 PMNs and fluid protein 2.7 g/dL. The rest of laboratories showed transaminitis with AST predominance, elevated BNP, and lymphopenia, normal ALP, platelets and TP/TTP.
Ceftriaxone 2 gr daily was empirically started. Abdominal ultrasound showed increased hepatic echotexture suggesting hepatocellular disease. Transthoracic echocardiogram showed an EF of 5% with severe biventricular dysfunction. Appropriate therapy for heart failure with reduced ejection fraction was started and the patient completed 7 days of antibiotic, showing significant improvement of symptoms without recurrence of ascites.
Discussion: This patient had risk factors for both hepatic and cardiac disease, with transaminases and ultrasound findings suggesting chronic liver damage, but BNP and echocardiogram suggesting acute exacerbated heart failure. Analyzing ascitic fluid helps determine its etiology. A SAAG ≥ 1.1 g/dL predicts portal hypertension; protein concentration < 2.5 g/dL correlates with liver-related ascites, whereas ≥ 2.5 g/dL, as seen on our patient, suggests a cardiac origin of ascites. A PMN count of ≥ 250/mm3 must be present to consider SBP.
Paracentesis is crucial in confirming or ruling out SBP, and delaying it is associated with increased mortality. Although this is an uncommon case, when presented with a patient with risk factors for multiple organ damage, one must always consider alternate causes and contributing factors for their symptoms. Regardless of its etiology, prompt initiation of empiric treatment remains mainstay in the treatment of SBP, however, treating the underlying cause decreases the chance of recurrence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jose Garcia-Corella indicated no relevant financial relationships.
Mahum Zahid indicated no relevant financial relationships.
Kevin Dao indicated no relevant financial relationships.
Leila Moosavi indicated no relevant financial relationships.
Ishaan Kalha indicated no relevant financial relationships.
Jose Garcia-Corella, MD, Mahum Zahid, MD, Kevin Dao, MD, Leila Moosavi, MD, Ishaan Kalha, MD. P1376 - A Rare Case of Spontaneous Bacterial Peritonitis in a Patient With Heart Failure and Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
