Sunday Poster Session
Category: Liver
P1387 - Blood Product Administration and Sodium Homeostasis in the Peri-Operative Liver Transplant Period
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Makeda Dawkins, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Makeda Dawkins, MD, Sanjeev Chugh, MD, MPH, David Spielvogel, MD,, Abhay Dhand, MD, Roxana Bodin, MD
Westchester Medical Center, Valhalla, NY
Introduction: Hypernatremia is uncommon in patients with decompensated cirrhosis, as most are volume-overloaded with hypervolemic hyponatremia due to splanchnic arterial vasodilation and portal hypertension. Blood transfusions are frequently required in these patients with compromised synthetic hepatic function, but may contain unphysiologically high sodium (Na) concentrations due to added preservatives (sodium citrate). We discuss a complex clinical case of severe hypernatremia associated with the use of fresh frozen plasma (FFP) during the peri-operative liver transplant period, highlighting challenges to maintaining sodium homeostasis with blood product transfusion, and the integral role of interdisciplinary collaboration for optimal decision-making.
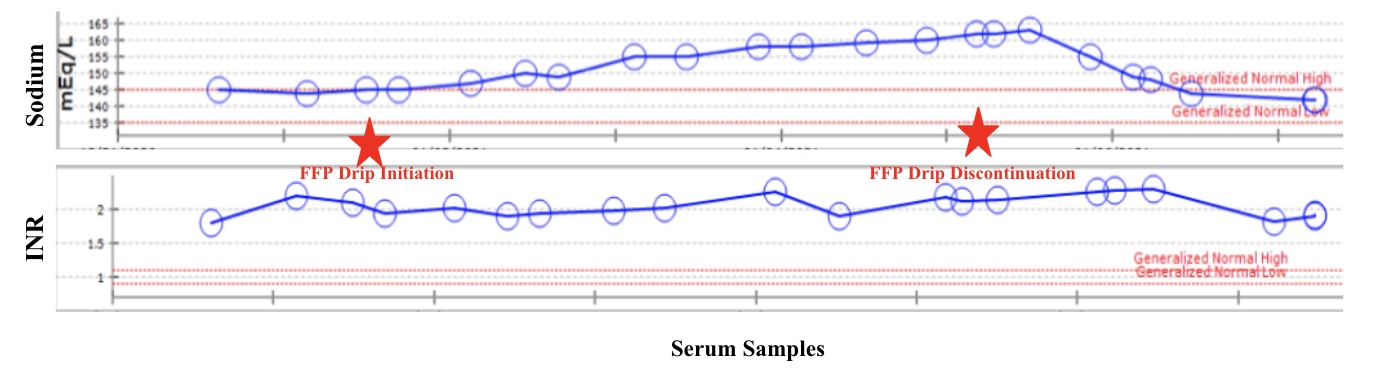
Case Description/Methods: A 44-year-old man with a history of decompensated cirrhosis underwent Surgical Aortic Valve Replacement (SAVR) for aortic insufficiency repair before liver transplantation (LT). He received transfusions of packed red blood cells and FFP preceding SAVR, with a goal hemoglobin >7g/dl and international normalized ratio (INR) < 2. Unable to achieve a post-SAVR INR < 2 using FFP transfusions, an FFP drip was initiated at a rate of 50cc/hour, and continued for five days. He subsequently developed severe progressive hypernatremia (peak Na 168 mmol/L), with a calculated free water deficit of 4.5L for target sodium of 150 mmol/L (wt: 86kg). Following interdisciplinary discussions with various care providers, FFP (which has a mean sodium concentration of 172 mEq/L) was discontinued. Intravenous dextrose 5% water was started with frequent free water boluses and tight glycemic control to avoid osmotic diuresis. Following resolution of his hypernatremia, he underwent liver transplantation without complication.
Discussion: Dysnatremias are common in patients with cirrhosis and those undergoing LT. Although infrequent, a strong association exists between pre-transplant hypernatremia, post-transplant survival, and 90-day in-hospital mortality even after adjusting for Model for End-Stage Liver Disease (MELD) score, with pre-transplant hypernatremia serving as a prognostic indicator for post-transplant morbidity and mortality. This case amplifies the need for evidence-based blood product administration in patients with advanced liver disease, highlighting secondary sodium disturbances due to positive solute balance, challenges to management, and potential post-transplant outcomes.
Disclosures:
Makeda Dawkins, MD, Sanjeev Chugh, MD, MPH, David Spielvogel, MD,, Abhay Dhand, MD, Roxana Bodin, MD. P1387 - Blood Product Administration and Sodium Homeostasis in the Peri-Operative Liver Transplant Period, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Hypernatremia is uncommon in patients with decompensated cirrhosis, as most are volume-overloaded with hypervolemic hyponatremia due to splanchnic arterial vasodilation and portal hypertension. Blood transfusions are frequently required in these patients with compromised synthetic hepatic function, but may contain unphysiologically high sodium (Na) concentrations due to added preservatives (sodium citrate). We discuss a complex clinical case of severe hypernatremia associated with the use of fresh frozen plasma (FFP) during the peri-operative liver transplant period, highlighting challenges to maintaining sodium homeostasis with blood product transfusion, and the integral role of interdisciplinary collaboration for optimal decision-making.
Case Description/Methods: A 44-year-old man with a history of decompensated cirrhosis underwent Surgical Aortic Valve Replacement (SAVR) for aortic insufficiency repair before liver transplantation (LT). He received transfusions of packed red blood cells and FFP preceding SAVR, with a goal hemoglobin >7g/dl and international normalized ratio (INR) < 2. Unable to achieve a post-SAVR INR < 2 using FFP transfusions, an FFP drip was initiated at a rate of 50cc/hour, and continued for five days. He subsequently developed severe progressive hypernatremia (peak Na 168 mmol/L), with a calculated free water deficit of 4.5L for target sodium of 150 mmol/L (wt: 86kg). Following interdisciplinary discussions with various care providers, FFP (which has a mean sodium concentration of 172 mEq/L) was discontinued. Intravenous dextrose 5% water was started with frequent free water boluses and tight glycemic control to avoid osmotic diuresis. Following resolution of his hypernatremia, he underwent liver transplantation without complication.
Discussion: Dysnatremias are common in patients with cirrhosis and those undergoing LT. Although infrequent, a strong association exists between pre-transplant hypernatremia, post-transplant survival, and 90-day in-hospital mortality even after adjusting for Model for End-Stage Liver Disease (MELD) score, with pre-transplant hypernatremia serving as a prognostic indicator for post-transplant morbidity and mortality. This case amplifies the need for evidence-based blood product administration in patients with advanced liver disease, highlighting secondary sodium disturbances due to positive solute balance, challenges to management, and potential post-transplant outcomes.
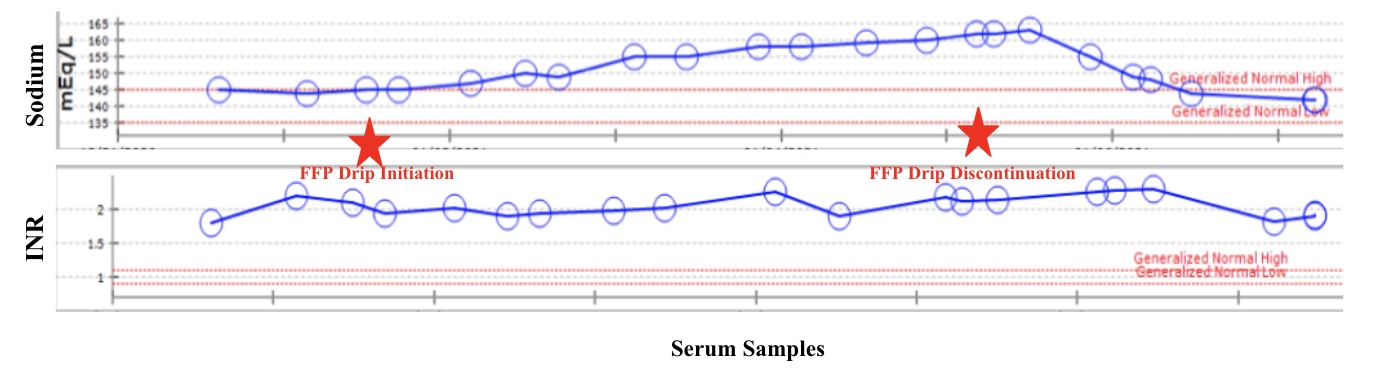
Figure: Figure 1: Trends in Serum Sodium and INR Pre- and Post- Fresh Frozen Plasma Drip Administration
Disclosures:
Makeda Dawkins indicated no relevant financial relationships.
Sanjeev Chugh indicated no relevant financial relationships.
David Spielvogel indicated no relevant financial relationships.
Abhay Dhand indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Makeda Dawkins, MD, Sanjeev Chugh, MD, MPH, David Spielvogel, MD,, Abhay Dhand, MD, Roxana Bodin, MD. P1387 - Blood Product Administration and Sodium Homeostasis in the Peri-Operative Liver Transplant Period, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
