Sunday Poster Session
Category: Liver
P1391 - Pylephlebitis as the Cause of Fulminant Hepatic Failure in a Young Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Daniel A. Guifarro, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Daniel A. Guifarro, MD1, Alejandro Nieto Dominguez, MD1, Chun-Wei Pan, MD1, Ambar Godoy, MD2, Gloria B.. Erazo, MD3, Carlos Avila, MD4
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Indiana University, Indianapolis, IN; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Yale New Haven Hospital, New Haven, CT
Introduction: Pylephlebitis is the infectious thrombophlebitis of the portal vein, it can present after an episode of appendicitis, diverticulitis, or peritonitis, although in some cases no previous infection can be identified. Treatment is usually with antibiotics; anticoagulation is only required in cases that are refractory to antibiotics, which are associated with thrombosis progression and hepatic complications.
Case Description/Methods: A 32-year-old migrant male with no medical history presents with intermittent right lower quadrant (RLQ) abdominal pain and fever for 3 days, with no radiation. Initial workup revealed mild hyperbilirubinemia to 4.5mg/dL, but no leukocytosis or any other abnormalities were noted. Abdominal ultrasound showed diffuse steatosis with patent hepatic vasculature and no dilation of the bile ducts; the patient was discharged home. He came back 8 days later presenting persistence of the symptoms, with jaundice and 10/10 RLQ abdominal pain, fever, and choluria. Work up showed Total Bilirubin:19.2 mg/dL, AST:277U/L, ALT:158U/L, GGT:204U/L, Alkaline Phosphatase: 242U/L, Albumin:2.9d/dL, WBC:12k/uL, PT:15.4s, PTT: 29.9s, INR:1.27. CT Abdomen showing near complete occlusion of the superior mesenteric artery and the portal vein and multiple areas of parenchymal focal hypoenhancement throughout the liver showing portal venous congestion. Endoscopic retrograde cholangiopancreatography was performed without abnormalities found; portal vein Doppler confirmed the portal vein thrombosis. Blood cultures grew E. coli; he was initially treated with ceftriaxone and metronidazole without improvement, then escalated to meropenem. Additionally, therapeutic anticoagulation with enoxaparin was started. General surgery had no existing surgical approach to attempt surgical thrombectomy in this patient; TIPS-thrombectomy was considered at this point and the patient was transferred to an outside hospital for evaluation for this procedure. He developed fulminant hepatic failure and worsening sepsis, passing away without undergoing the procedure.
Discussion: Pylephlebitis is a rare condition that still presents high mortality to this day (14-19% of cases), with multiple factors that can influence disease progression and affect patient outcomes, including factors leading to delayed care, bacterial resistance, and no response to anticoagulation. It is important to have an early intervention with antibiotics and to consider the need to escalate therapy with anticoagulation or even thrombectomy when necessary.

Disclosures:
Daniel A. Guifarro, MD1, Alejandro Nieto Dominguez, MD1, Chun-Wei Pan, MD1, Ambar Godoy, MD2, Gloria B.. Erazo, MD3, Carlos Avila, MD4. P1391 - Pylephlebitis as the Cause of Fulminant Hepatic Failure in a Young Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Indiana University, Indianapolis, IN; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Yale New Haven Hospital, New Haven, CT
Introduction: Pylephlebitis is the infectious thrombophlebitis of the portal vein, it can present after an episode of appendicitis, diverticulitis, or peritonitis, although in some cases no previous infection can be identified. Treatment is usually with antibiotics; anticoagulation is only required in cases that are refractory to antibiotics, which are associated with thrombosis progression and hepatic complications.
Case Description/Methods: A 32-year-old migrant male with no medical history presents with intermittent right lower quadrant (RLQ) abdominal pain and fever for 3 days, with no radiation. Initial workup revealed mild hyperbilirubinemia to 4.5mg/dL, but no leukocytosis or any other abnormalities were noted. Abdominal ultrasound showed diffuse steatosis with patent hepatic vasculature and no dilation of the bile ducts; the patient was discharged home. He came back 8 days later presenting persistence of the symptoms, with jaundice and 10/10 RLQ abdominal pain, fever, and choluria. Work up showed Total Bilirubin:19.2 mg/dL, AST:277U/L, ALT:158U/L, GGT:204U/L, Alkaline Phosphatase: 242U/L, Albumin:2.9d/dL, WBC:12k/uL, PT:15.4s, PTT: 29.9s, INR:1.27. CT Abdomen showing near complete occlusion of the superior mesenteric artery and the portal vein and multiple areas of parenchymal focal hypoenhancement throughout the liver showing portal venous congestion. Endoscopic retrograde cholangiopancreatography was performed without abnormalities found; portal vein Doppler confirmed the portal vein thrombosis. Blood cultures grew E. coli; he was initially treated with ceftriaxone and metronidazole without improvement, then escalated to meropenem. Additionally, therapeutic anticoagulation with enoxaparin was started. General surgery had no existing surgical approach to attempt surgical thrombectomy in this patient; TIPS-thrombectomy was considered at this point and the patient was transferred to an outside hospital for evaluation for this procedure. He developed fulminant hepatic failure and worsening sepsis, passing away without undergoing the procedure.
Discussion: Pylephlebitis is a rare condition that still presents high mortality to this day (14-19% of cases), with multiple factors that can influence disease progression and affect patient outcomes, including factors leading to delayed care, bacterial resistance, and no response to anticoagulation. It is important to have an early intervention with antibiotics and to consider the need to escalate therapy with anticoagulation or even thrombectomy when necessary.

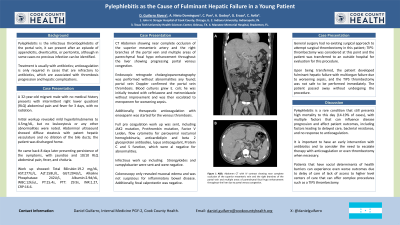
Figure: Abdomen CT with IV contrast showing near complete occlusion of the superior mesenteric artery and the portal vein and multiple areas of parenchymal focal hypoenhancement throughout the liver due to portal venous congestion.
Disclosures:
Daniel Guifarro indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Ambar Godoy indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Carlos Avila indicated no relevant financial relationships.
Daniel A. Guifarro, MD1, Alejandro Nieto Dominguez, MD1, Chun-Wei Pan, MD1, Ambar Godoy, MD2, Gloria B.. Erazo, MD3, Carlos Avila, MD4. P1391 - Pylephlebitis as the Cause of Fulminant Hepatic Failure in a Young Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
