Sunday Poster Session
Category: Liver
P1397 - From GERD to Emergency: The Hidden Peril of Spontaneous Liver Laceration
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Isabella Suarez Alcala, MD
Palmetto General Hospital
Hialeah, FL
Presenting Author(s)
Isabella Suarez Alcala, MD1, Hira Chaudhary, DO2, Frances M. Lugo Jimenez, MD1
1Palmetto General Hospital, Hialeah, FL; 2Palmetto General Hospital, Pembroke Pines, FL
Introduction: Spontaneous liver laceration is a rare and potentially life-threatening condition, typically occurring in the absence of trauma. Common causes include HELLP syndrome, liver neoplasms, vasculitides, coagulopathy, and in exceptional cases, the cause remains idiopathic. We present the case of a patient with abdominal pain initially attributed to gastroesophageal reflux disease (GERD), who was subsequently diagnosed with a spontaneous liver laceration.
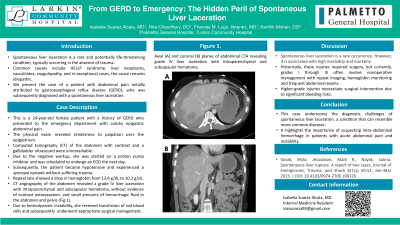
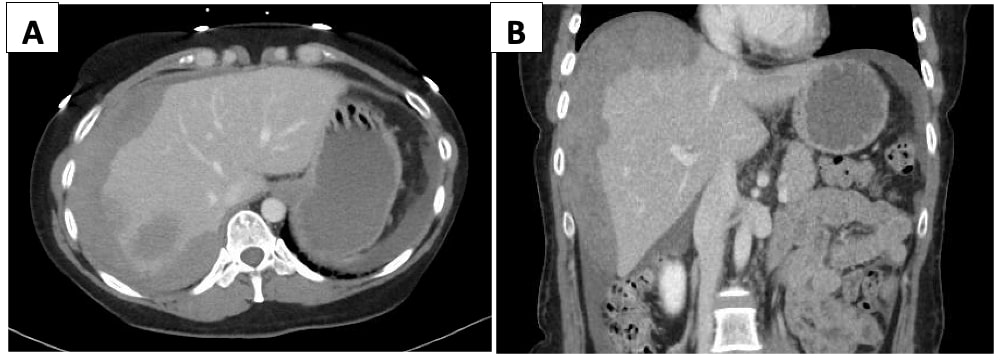
Case Description/Methods: This is a 24-year-old female patient with a medical history of GERD who presented to the emergency department with colicky epigastric abdominal pain that started the day prior. The pain was rated 8/10 in intensity, radiated to the right upper quadrant and right shoulder, unrelated to food intake, and associated with nausea, dyspnea, and a presyncopal episode. She denied previous esophagogastroduodenoscopy (EGD). Upon arrival, she was hemodynamically stable. The physical exam revealed tenderness to palpation over the epigastrium. Computed tomography (CT) of the abdomen with contrast and a gallbladder ultrasound were unremarkable. Due to the negative workup, she was started on a proton pump inhibitor and was scheduled to undergo an EGD the next day. However, overnight, the patient became hypotensive and experienced a syncopal episode without suffering trauma. Repeat labs showed a drop in hemoglobin from 13.8 g/dL to 10.3 g/dL. CT angiography of the abdomen revealed a grade IV liver laceration with intraparenchymal and subcapsular hematoma, without evidence of contrast extravasation, and small amounts of hemorrhagic fluid in the abdomen and pelvis (Fig.1). Due to hemodynamic instability, she received two units of red blood cells and was subsequently transferred to a trauma center for appropriate surgical management.
Discussion: This case underscores the diagnostic challenges of spontaneous liver laceration, a condition that can resemble more common diseases. The Association for the Surgery of Trauma (AAST) categorizes liver injuries into six grades. Historically, these injuries required surgery, but currently, grades I through III often involve nonoperative management with repeat imaging, hemoglobin monitoring and frequent abdominal exams. Higher-grade injuries, like in our patient's grade IV, necessitate surgical intervention due to significant bleeding risks. This highlights the importance of suspecting intra-abdominal hemorrhage in patients with acute abdominal pain and instability.
Disclosures:
Isabella Suarez Alcala, MD1, Hira Chaudhary, DO2, Frances M. Lugo Jimenez, MD1. P1397 - From GERD to Emergency: The Hidden Peril of Spontaneous Liver Laceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Palmetto General Hospital, Hialeah, FL; 2Palmetto General Hospital, Pembroke Pines, FL
Introduction: Spontaneous liver laceration is a rare and potentially life-threatening condition, typically occurring in the absence of trauma. Common causes include HELLP syndrome, liver neoplasms, vasculitides, coagulopathy, and in exceptional cases, the cause remains idiopathic. We present the case of a patient with abdominal pain initially attributed to gastroesophageal reflux disease (GERD), who was subsequently diagnosed with a spontaneous liver laceration.
Case Description/Methods: This is a 24-year-old female patient with a medical history of GERD who presented to the emergency department with colicky epigastric abdominal pain that started the day prior. The pain was rated 8/10 in intensity, radiated to the right upper quadrant and right shoulder, unrelated to food intake, and associated with nausea, dyspnea, and a presyncopal episode. She denied previous esophagogastroduodenoscopy (EGD). Upon arrival, she was hemodynamically stable. The physical exam revealed tenderness to palpation over the epigastrium. Computed tomography (CT) of the abdomen with contrast and a gallbladder ultrasound were unremarkable. Due to the negative workup, she was started on a proton pump inhibitor and was scheduled to undergo an EGD the next day. However, overnight, the patient became hypotensive and experienced a syncopal episode without suffering trauma. Repeat labs showed a drop in hemoglobin from 13.8 g/dL to 10.3 g/dL. CT angiography of the abdomen revealed a grade IV liver laceration with intraparenchymal and subcapsular hematoma, without evidence of contrast extravasation, and small amounts of hemorrhagic fluid in the abdomen and pelvis (Fig.1). Due to hemodynamic instability, she received two units of red blood cells and was subsequently transferred to a trauma center for appropriate surgical management.
Discussion: This case underscores the diagnostic challenges of spontaneous liver laceration, a condition that can resemble more common diseases. The Association for the Surgery of Trauma (AAST) categorizes liver injuries into six grades. Historically, these injuries required surgery, but currently, grades I through III often involve nonoperative management with repeat imaging, hemoglobin monitoring and frequent abdominal exams. Higher-grade injuries, like in our patient's grade IV, necessitate surgical intervention due to significant bleeding risks. This highlights the importance of suspecting intra-abdominal hemorrhage in patients with acute abdominal pain and instability.
Figure: Figure 1: Axial (A) and coronal (B) planes of abdominal CTA revealing grade IV liver laceration with intraparenchymal and subcapsular hematoma.
Disclosures:
Isabella Suarez Alcala indicated no relevant financial relationships.
Hira Chaudhary indicated no relevant financial relationships.
Frances Lugo Jimenez indicated no relevant financial relationships.
Isabella Suarez Alcala, MD1, Hira Chaudhary, DO2, Frances M. Lugo Jimenez, MD1. P1397 - From GERD to Emergency: The Hidden Peril of Spontaneous Liver Laceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
