Sunday Poster Session
Category: Liver
P1403 - A Clinical Puzzle: A Case of Vanishing Bile Duct Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Swati Mahapatra, DO
TTUHSC
El Paso, TX
Presenting Author(s)
Swati Mahapatra, DO1, Hesham Elgouhari, MD2, Shivangini Duggal, MD3, Akanksha Togra, MD1, Attilio Orazi, MD4, Jonathan L. Lavezo, MD4, Marc Zuckerman, MD1, Sherif E.. Elhanafi, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texoma Liver Center, Denison, TX; 3TTUHSC, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Vanishing bile duct syndrome (VBDS) is an uncommon and severe condition characterized by the progressive destruction of intrahepatic bile ducts, resulting in cholestasis and liver dysfunction. VBDS is classically attributed to drug toxicity, immunologic disorders, infections, and neoplastic disorders. We present a case of VBDS with a rarely described association.
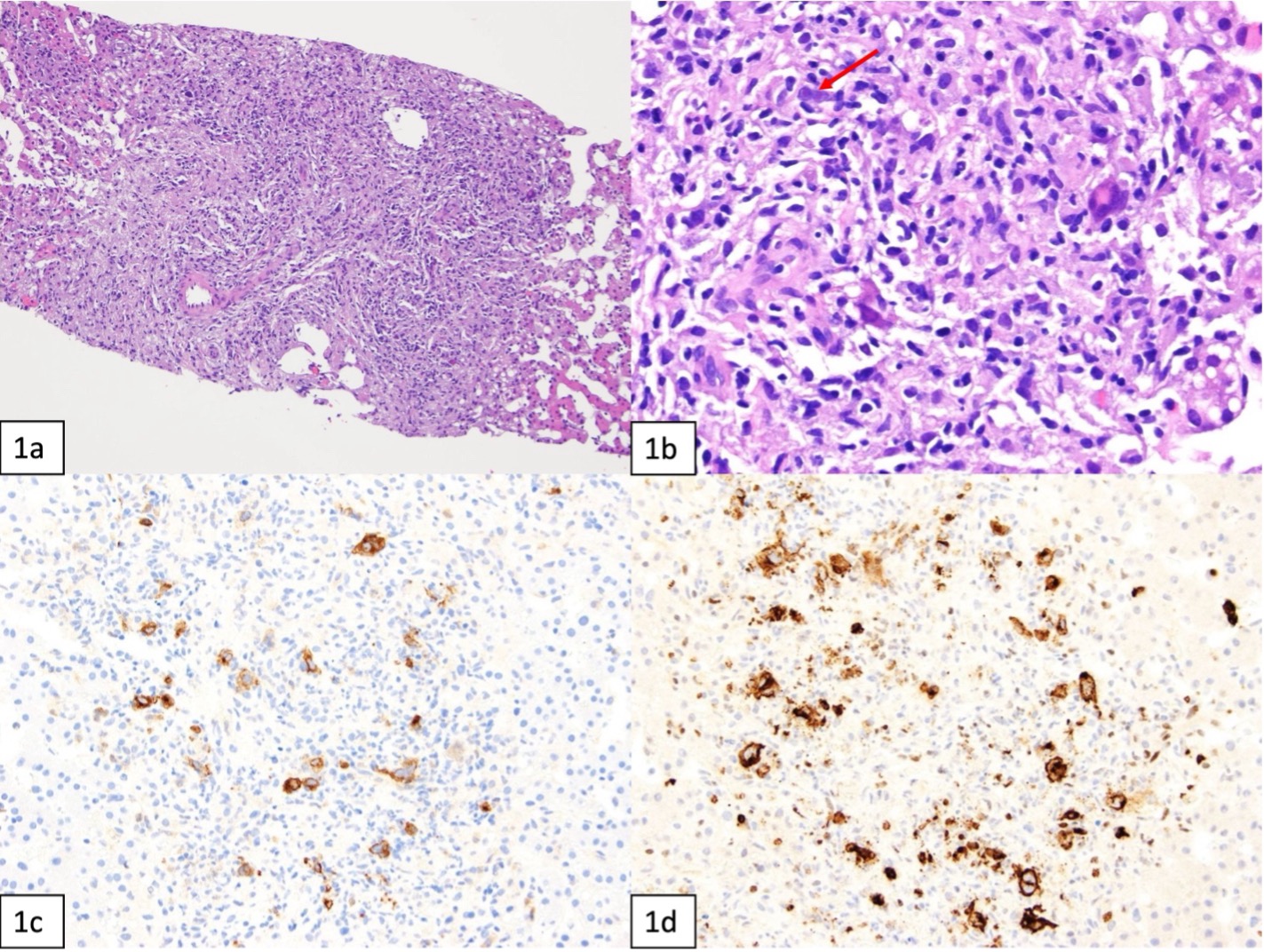
Case Description/Methods: A previously healthy 24-year-old male presented to the emergency department with fatigue, abdominal pain, subjective fevers and jaundice for the past two weeks. He denied recent travel, alcohol, smoking, illicit drugs, herbal or prescribed medication use. On arrival, patient was febrile and tachycardic. Labs were notable for elevated total bilirubin at 10.6, direct bilirubin 5.6, elevated alkaline phosphatase at 1048, AST 89, ALT 84, LDH of 379, INR of 1.4 and platelets of 259. An extensive liver and infectious workup were negative. MRI/MRCP was obtained to rule out an obstructive etiology and revealed hepatomegaly with inhomogeneous fatty infiltration of the liver along with heterogenous enhancement of the spleen which raised the possibility of lymphoproliferative disorder with no concern for biliary obstruction or cholangitis. Due to these findings, a liver biopsy was performed which revealed hepatic parenchyma with an inflammatory infiltrate in the portal tracts and bile duct loss, raising suspicion for VBDS. Further special staining was requested. CT chest and neck were ordered to assess for lymphadenopathy. CT chest was unremarkable; however, the CT neck showed small cervical lymphadenopathy. Further staining of the liver biopsy revealed large, atypical CD30 positive cells highly suspicious for HL. The lymph node biopsy was also performed which further supported the diagnosis of classical HL. At this point, Stage IV Classical HL nodular sclerosis subtype was confirmed, and inpatient chemotherapy was started. Patient was successfully discharged with outpatient chemotherapy.
Discussion: The intricacies between VBDS and HL present a diagnostic dilemma as illustrated here. This case highlights the importance of considering infiltrative lymphoproliferative disease as a potential cause of VBDS and cholestasis in the setting of an otherwise negative workup. Timely recognition of this relationship is crucial for initiating interventions to improve patient outcomes and quality of life.
Disclosures:
Swati Mahapatra, DO1, Hesham Elgouhari, MD2, Shivangini Duggal, MD3, Akanksha Togra, MD1, Attilio Orazi, MD4, Jonathan L. Lavezo, MD4, Marc Zuckerman, MD1, Sherif E.. Elhanafi, MD1. P1403 - A Clinical Puzzle: A Case of Vanishing Bile Duct Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texoma Liver Center, Denison, TX; 3TTUHSC, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Vanishing bile duct syndrome (VBDS) is an uncommon and severe condition characterized by the progressive destruction of intrahepatic bile ducts, resulting in cholestasis and liver dysfunction. VBDS is classically attributed to drug toxicity, immunologic disorders, infections, and neoplastic disorders. We present a case of VBDS with a rarely described association.
Case Description/Methods: A previously healthy 24-year-old male presented to the emergency department with fatigue, abdominal pain, subjective fevers and jaundice for the past two weeks. He denied recent travel, alcohol, smoking, illicit drugs, herbal or prescribed medication use. On arrival, patient was febrile and tachycardic. Labs were notable for elevated total bilirubin at 10.6, direct bilirubin 5.6, elevated alkaline phosphatase at 1048, AST 89, ALT 84, LDH of 379, INR of 1.4 and platelets of 259. An extensive liver and infectious workup were negative. MRI/MRCP was obtained to rule out an obstructive etiology and revealed hepatomegaly with inhomogeneous fatty infiltration of the liver along with heterogenous enhancement of the spleen which raised the possibility of lymphoproliferative disorder with no concern for biliary obstruction or cholangitis. Due to these findings, a liver biopsy was performed which revealed hepatic parenchyma with an inflammatory infiltrate in the portal tracts and bile duct loss, raising suspicion for VBDS. Further special staining was requested. CT chest and neck were ordered to assess for lymphadenopathy. CT chest was unremarkable; however, the CT neck showed small cervical lymphadenopathy. Further staining of the liver biopsy revealed large, atypical CD30 positive cells highly suspicious for HL. The lymph node biopsy was also performed which further supported the diagnosis of classical HL. At this point, Stage IV Classical HL nodular sclerosis subtype was confirmed, and inpatient chemotherapy was started. Patient was successfully discharged with outpatient chemotherapy.
Discussion: The intricacies between VBDS and HL present a diagnostic dilemma as illustrated here. This case highlights the importance of considering infiltrative lymphoproliferative disease as a potential cause of VBDS and cholestasis in the setting of an otherwise negative workup. Timely recognition of this relationship is crucial for initiating interventions to improve patient outcomes and quality of life.
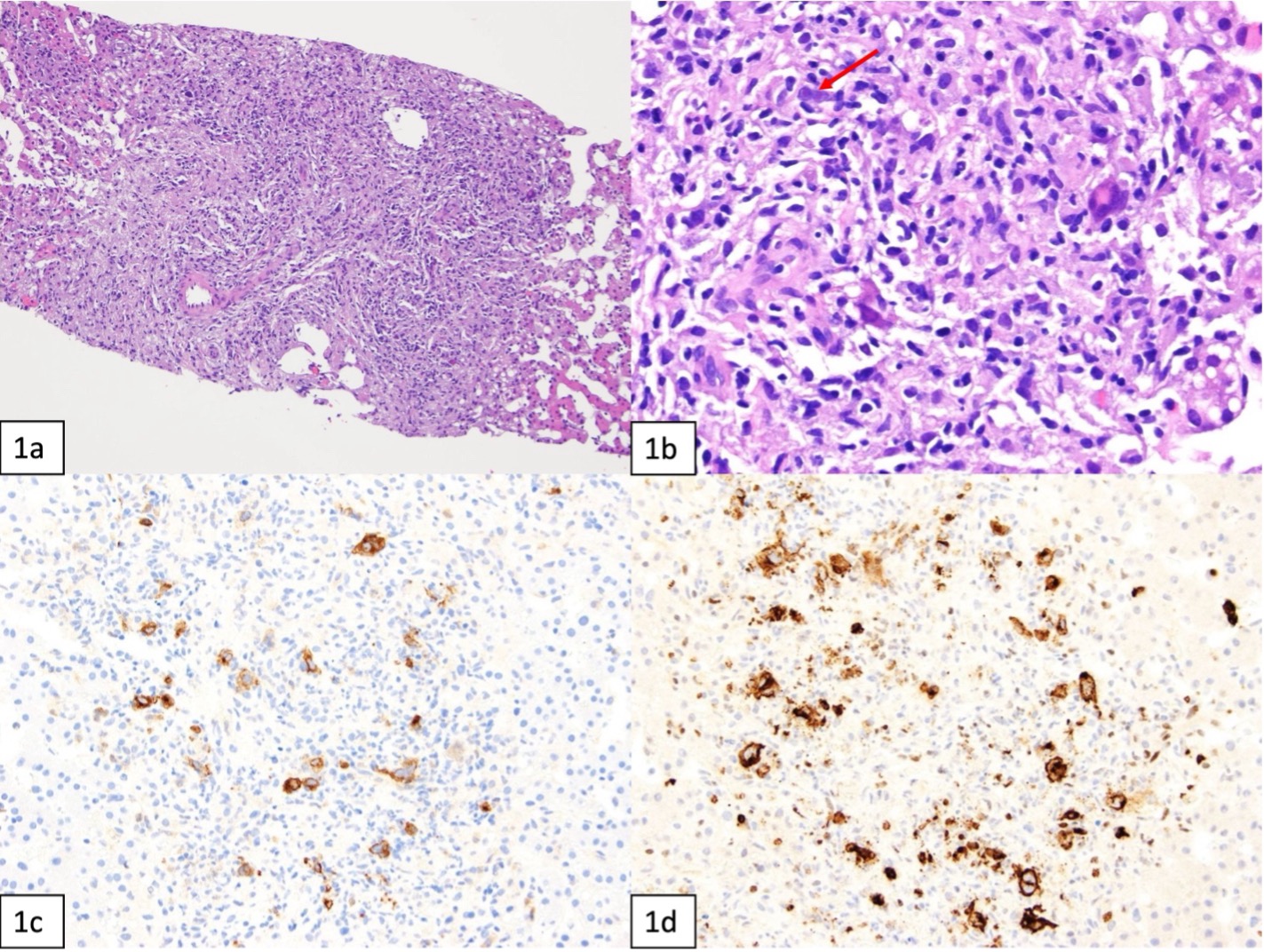
Figure: Portal tract showing an abnormal lymphoid proliferation with scattered Hodgkin-Reed-Sternberg cells both of the classical (red arrow) and lacunar cell type surrounded by small lymphocytes and other non neoplastic inflammatory cells (1a 100x, 1b 200x). Hodgkin-Reed-Sternberg cells show CD30 (1c 200x) and CD15 (1d 200x) expression by immunohistochemical stains, consistent with Hodgkin lymphoma.
Disclosures:
Swati Mahapatra indicated no relevant financial relationships.
Hesham Elgouhari indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Akanksha Togra: Clinexel Inc – Owner/Ownership Interest. Clinexel Life Sciences Pvt Ltd – Owner/Ownership Interest. Cytenet Life science LLP – Owner/Ownership Interest. GLRK Healthcare foundation (Non-profit Organization Company) – Owner/Ownership Interest.
Attilio Orazi indicated no relevant financial relationships.
Jonathan Lavezo indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Swati Mahapatra, DO1, Hesham Elgouhari, MD2, Shivangini Duggal, MD3, Akanksha Togra, MD1, Attilio Orazi, MD4, Jonathan L. Lavezo, MD4, Marc Zuckerman, MD1, Sherif E.. Elhanafi, MD1. P1403 - A Clinical Puzzle: A Case of Vanishing Bile Duct Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

