Sunday Poster Session
Category: Liver
P1404 - The First Documented Case of Ileocolic Anastomotic Varices
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

David Braun, MD
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
David Salus Braun, MD1, Kyle Schneider, MD1, Parvez Mantry, MD2
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Liver Institute, Dallas, TX
Introduction: Ectopic varices (EV) are dilated portosystemic collateral veins located at sites other than the gastroesophageal region. EV account for 1-5% of variceal bleeding in patients with cirrhosis and 20-30% of variceal bleeding in patients with extrahepatic portal hypertension. Anastomotic varices (AV) are a subset of EV that are seen most commonly in the jejunum and ileum. AV at locations outside the small intestine are exceedingly rare; this is the first documented case of AV located at an ileocolic anastomosis (ICA).
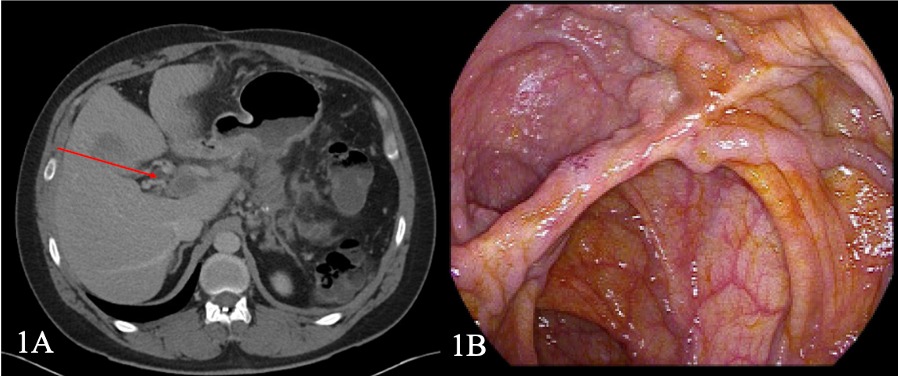
Case Description/Methods: A 38-year-old male was evaluated for a three-week history of hematochezia. Medical history was significant for acute alcoholic pancreatitis (AP) seven years earlier, complicated by compartment syndrome necessitating exploratory laparotomy (EL) with hemicolectomy and ICA. AP was also complicated by pseudocysts requiring cystgastrostomy and eventual distal pancreatectomy and splenectomy due to pancreatic duct transection. He had been abstinent from alcohol since the initial episode of AP. Physical exam revealed a heart rate of 110 beats per minute and bright red blood in the rectal vault. Lab results were notable for hemoglobin 8.4 g/dL and platelets 1,045 (x 103U/L), both of which were normal one year earlier. Ceftriaxone, high-dose proton pump inhibitor and an octreotide drip were initiated; hydroxyurea was added for thrombocytosis secondary to splenectomy. Computed tomography showed a slightly nodular liver and an occlusive portal vein thrombus extending to the superior mesenteric vein (SMV) with cavernous transformation (Fig 1A). Upper endoscopy was normal; colonoscopy revealed large varices at the ICA without active bleeding (Fig 1B). Transjugular intrahepatic portosystemic shunt was contraindicated due to clot burden; a heparin drip was initiated. The patient subsequently underwent an EL with SMV thrombectomy, lysis of adhesions, resection of ICA with varices and new side-to-side ICA. The patient had an uncomplicated post-operative course and has not had any further episodes of bleeding.
Discussion: While previous cases of AV at esophagojejunal, gastroduodenal, and colorectal anastomoses have been described, this is the first documented case of ileocolic AV. AV pose numerous clinical challenges as they are often difficult to localize and no clear treatment guidelines exist. After resuscitation, endoscopic therapy should be attempted; if unsuccessful, patients should be promptly referred to interventional radiology or surgery for definitive management.
Disclosures:
David Salus Braun, MD1, Kyle Schneider, MD1, Parvez Mantry, MD2. P1404 - The First Documented Case of Ileocolic Anastomotic Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Liver Institute, Dallas, TX
Introduction: Ectopic varices (EV) are dilated portosystemic collateral veins located at sites other than the gastroesophageal region. EV account for 1-5% of variceal bleeding in patients with cirrhosis and 20-30% of variceal bleeding in patients with extrahepatic portal hypertension. Anastomotic varices (AV) are a subset of EV that are seen most commonly in the jejunum and ileum. AV at locations outside the small intestine are exceedingly rare; this is the first documented case of AV located at an ileocolic anastomosis (ICA).
Case Description/Methods: A 38-year-old male was evaluated for a three-week history of hematochezia. Medical history was significant for acute alcoholic pancreatitis (AP) seven years earlier, complicated by compartment syndrome necessitating exploratory laparotomy (EL) with hemicolectomy and ICA. AP was also complicated by pseudocysts requiring cystgastrostomy and eventual distal pancreatectomy and splenectomy due to pancreatic duct transection. He had been abstinent from alcohol since the initial episode of AP. Physical exam revealed a heart rate of 110 beats per minute and bright red blood in the rectal vault. Lab results were notable for hemoglobin 8.4 g/dL and platelets 1,045 (x 103U/L), both of which were normal one year earlier. Ceftriaxone, high-dose proton pump inhibitor and an octreotide drip were initiated; hydroxyurea was added for thrombocytosis secondary to splenectomy. Computed tomography showed a slightly nodular liver and an occlusive portal vein thrombus extending to the superior mesenteric vein (SMV) with cavernous transformation (Fig 1A). Upper endoscopy was normal; colonoscopy revealed large varices at the ICA without active bleeding (Fig 1B). Transjugular intrahepatic portosystemic shunt was contraindicated due to clot burden; a heparin drip was initiated. The patient subsequently underwent an EL with SMV thrombectomy, lysis of adhesions, resection of ICA with varices and new side-to-side ICA. The patient had an uncomplicated post-operative course and has not had any further episodes of bleeding.
Discussion: While previous cases of AV at esophagojejunal, gastroduodenal, and colorectal anastomoses have been described, this is the first documented case of ileocolic AV. AV pose numerous clinical challenges as they are often difficult to localize and no clear treatment guidelines exist. After resuscitation, endoscopic therapy should be attempted; if unsuccessful, patients should be promptly referred to interventional radiology or surgery for definitive management.
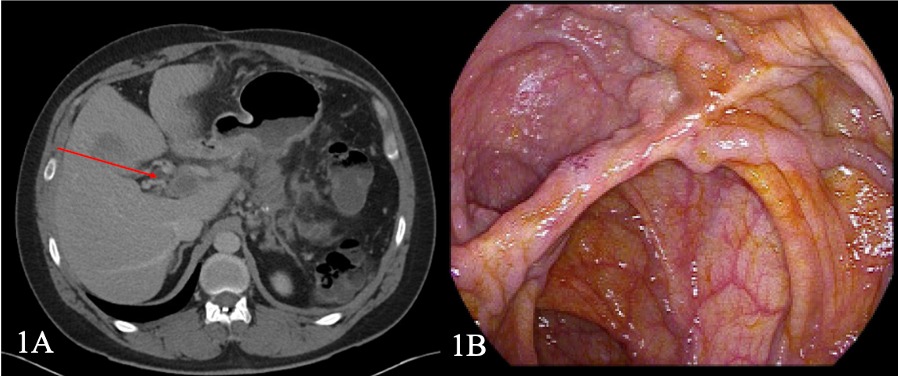
Figure: Fig 1. (A) Computed tomography showing large portal vein thrombus extending to the superior mesenteric vein with cavernous transformation and (B) Endoscopic view of large, non-bleeding varices at the ileocolic anastomosis.
Disclosures:
David Salus Braun indicated no relevant financial relationships.
Kyle Schneider indicated no relevant financial relationships.
Parvez Mantry indicated no relevant financial relationships.
David Salus Braun, MD1, Kyle Schneider, MD1, Parvez Mantry, MD2. P1404 - The First Documented Case of Ileocolic Anastomotic Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

