Sunday Poster Session
Category: Liver
P1408 - Cholangitis Lenta and Giant Cell Hepatitis: A Unique Coexistence
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Anirudha Chatterjee, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Anirudha Chatterjee, MD1, Shiv Patel, BSA2, Jordan Malone, DO1, Rebecca Sullivan, MD1, Reuben Powell, MD1, Celeste Wagner, MD1, Abdullah Muftah, MD1, Heather Stevenson, MD, PhD1, Kashif Khan, MD1
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
Introduction: Cholangitis lenta (CL) is a rare histopathological diagnosis characterized by dilated bile ductules containing inspissated bile, often associated with high bilirubin levels. Most cases have been observed in patients with clinical evidence of sepsis or a history of liver transplantation. Giant cell hepatitis (GCH) almost exclusively presents in children and is characterized by inflammation and large multinucleated hepatocytes in the hepatic parenchyma. Both conditions are diagnosed via liver biopsy. We present a case of an elderly man with decompensated cirrhosis secondary to autoimmune hepatitis (AIH) who was found to have biopsy-proven CL and GCH.
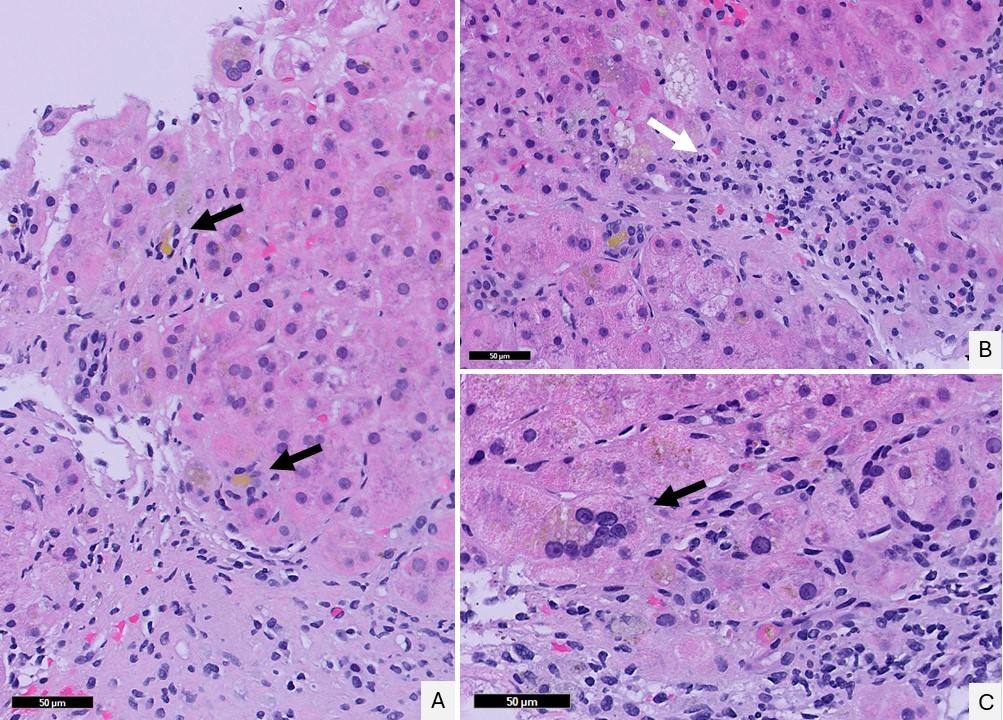
Case Description/Methods: A 70-year-old man with a history of AIH maintained on azathioprine (AZA) presented with jaundice, ascites, and lower-extremity edema. Labs revealed elevated aminotransferase levels ( >1000) and severe hyperbilirubinemia ( >20). The patient was treated for an acute AIH flare with prednisone in addition to AZA. He improved clinically, his liver chemistries improved, and he was discharged. He was readmitted for acute variceal bleeding and underwent a transjugular intrahepatic portosystemic shunt (TIPS) placement. Following discharge, he was readmitted for altered mental status, which improved after treatment was initiated for hepatic encephalopathy. Urine culture was drawn and returned positive for Pseudomonas aeruginosa. He was treated with ciprofloxacin for a urinary tract infection not complicated by sepsis. Given his slowly declining clinical condition and persistently elevated bilirubin levels, a liver biopsy was performed to assess disease activity. Biopsy results revealed substantially decreased active lobular inflammation compared to a previous biopsy from 6 years prior but showed the development of inspissated bile within ducts consistent with CL and the development of giant cell transformation consistent with GCH. Given his poor prognosis and declining functional status, palliative care was consulted, and the patient elected to transition to hospice care, where he ultimately passed away.
Discussion: This case highlights the potential for two rare conditions to occur simultaneously in an atypical patient. Given the high mortality rates associated with both CL and GCH, it is crucial to consider these diagnoses as part of the differential and to promptly initiate work-up when encountering worsening hepatic decompensation in the setting of autoimmune liver diseases such as AIH.
Disclosures:
Anirudha Chatterjee, MD1, Shiv Patel, BSA2, Jordan Malone, DO1, Rebecca Sullivan, MD1, Reuben Powell, MD1, Celeste Wagner, MD1, Abdullah Muftah, MD1, Heather Stevenson, MD, PhD1, Kashif Khan, MD1. P1408 - Cholangitis Lenta and Giant Cell Hepatitis: A Unique Coexistence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
Introduction: Cholangitis lenta (CL) is a rare histopathological diagnosis characterized by dilated bile ductules containing inspissated bile, often associated with high bilirubin levels. Most cases have been observed in patients with clinical evidence of sepsis or a history of liver transplantation. Giant cell hepatitis (GCH) almost exclusively presents in children and is characterized by inflammation and large multinucleated hepatocytes in the hepatic parenchyma. Both conditions are diagnosed via liver biopsy. We present a case of an elderly man with decompensated cirrhosis secondary to autoimmune hepatitis (AIH) who was found to have biopsy-proven CL and GCH.
Case Description/Methods: A 70-year-old man with a history of AIH maintained on azathioprine (AZA) presented with jaundice, ascites, and lower-extremity edema. Labs revealed elevated aminotransferase levels ( >1000) and severe hyperbilirubinemia ( >20). The patient was treated for an acute AIH flare with prednisone in addition to AZA. He improved clinically, his liver chemistries improved, and he was discharged. He was readmitted for acute variceal bleeding and underwent a transjugular intrahepatic portosystemic shunt (TIPS) placement. Following discharge, he was readmitted for altered mental status, which improved after treatment was initiated for hepatic encephalopathy. Urine culture was drawn and returned positive for Pseudomonas aeruginosa. He was treated with ciprofloxacin for a urinary tract infection not complicated by sepsis. Given his slowly declining clinical condition and persistently elevated bilirubin levels, a liver biopsy was performed to assess disease activity. Biopsy results revealed substantially decreased active lobular inflammation compared to a previous biopsy from 6 years prior but showed the development of inspissated bile within ducts consistent with CL and the development of giant cell transformation consistent with GCH. Given his poor prognosis and declining functional status, palliative care was consulted, and the patient elected to transition to hospice care, where he ultimately passed away.
Discussion: This case highlights the potential for two rare conditions to occur simultaneously in an atypical patient. Given the high mortality rates associated with both CL and GCH, it is crucial to consider these diagnoses as part of the differential and to promptly initiate work-up when encountering worsening hepatic decompensation in the setting of autoimmune liver diseases such as AIH.
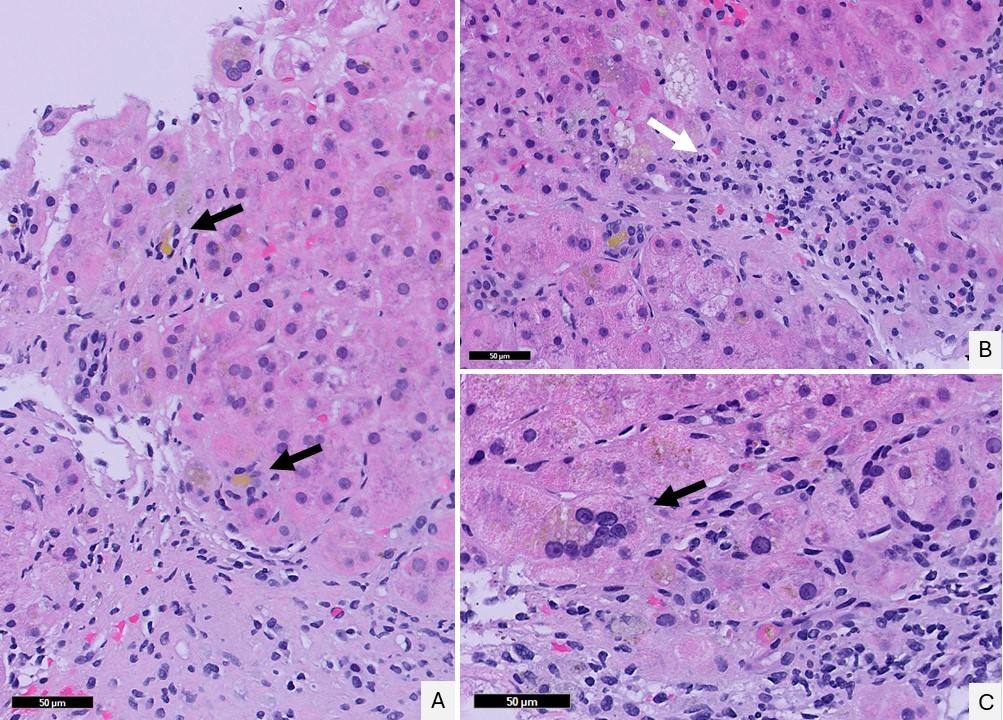
Figure: A: Periportal proliferation of dilated bile ductules containing inspissated bile with occasional neutrophils (black arrows). [H&E 40X]
B: Portal tract showing minimal-to-mild lymphoplasmacytic inflammation (white arrow). [H&E 40X]
C: Multinucleated giant cell (black arrow). [H&E 40X]
B: Portal tract showing minimal-to-mild lymphoplasmacytic inflammation (white arrow). [H&E 40X]
C: Multinucleated giant cell (black arrow). [H&E 40X]
Disclosures:
Anirudha Chatterjee indicated no relevant financial relationships.
Shiv Patel indicated no relevant financial relationships.
Jordan Malone indicated no relevant financial relationships.
Rebecca Sullivan indicated no relevant financial relationships.
Reuben Powell indicated no relevant financial relationships.
Celeste Wagner indicated no relevant financial relationships.
Abdullah Muftah indicated no relevant financial relationships.
Heather Stevenson indicated no relevant financial relationships.
Kashif Khan indicated no relevant financial relationships.
Anirudha Chatterjee, MD1, Shiv Patel, BSA2, Jordan Malone, DO1, Rebecca Sullivan, MD1, Reuben Powell, MD1, Celeste Wagner, MD1, Abdullah Muftah, MD1, Heather Stevenson, MD, PhD1, Kashif Khan, MD1. P1408 - Cholangitis Lenta and Giant Cell Hepatitis: A Unique Coexistence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
