Sunday Poster Session
Category: Liver
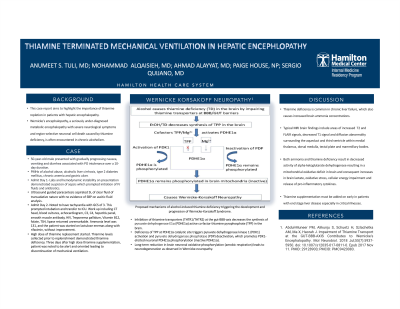
P1414 - Thiamine Terminated Mechanical Ventilation in Hepatic Encephalopathy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Anumeet S. Tuli, MD, MBBS
Hamilton Medical Center
Dalton, GA
Presenting Author(s)
Anumeet S. Tuli, MD, MBBS1, Mohammad Alqaisieh, MD1, Ahmad Alayyat, MD1, Sergio Quijano, MD2, Paige House, NP1
1Hamilton Medical Center, Dalton, GA; 2Hamilton Health Care System, Dalton, GA
Introduction: Thiamine deficiency is common in chronic liver failure, which also causes increased brain ammonia concentrations. Both ammonia and thiamine deficiency result in decreased activity of alpha-ketoglutarate dehydrogenase resulting in a mitochondrial oxidative deficit in brain and consequent increases in brain lactate, oxidative stress, cellular energy impairment and release of pro-inflammatory cytokines.
Case Description/Methods: 50-year-old male with PMHx of alcoholic liver cirrhosis, chronic anemia, type 2 diabetes mellitus, alcohol abuse and gastric ulcer presented with chief complaints of nausea, vomiting and diarrhea of 10 days duration associated with inability of tolerating oral intake. Last alcohol use 2 weeks ago. Vitals stable on room air, alert and oriented to time, place, person and situation.
IV fluids and broad-spectrum antibiotics were started to treat acute kidney injury and suspected sepsis, given the markedly elevated WBC of 25000/mcL and lactic acid of 5.1 mmol/L. Ultrasound guided paracentesis aspirated 5L of clear fluid of transudative nature with no evidence of SBP.
On the second day of admission, patient noted to have tachycardia with GCS of 3. This prompted intubation and transfer to ICU. Work up including CT head, blood cultures, echocardiogram, C3, C4, hepatitis panel, smooth muscle antibody, HIV, Treponema pallidum, Vitamin B12, folate, TSH, lipase returned unremarkable. Ammonia level was 131, and the patient was started on lactulose enemas along with Rifaximin, without improvement for two days. Patient was then started on high dose of thiamine. Thiamine levels collected prior to replenishment demonstrated thiamine deficiency (Image 1). Three days after high dose thiamine supplementation, patient was noted to be alert and oriented leading to discontinuation of mechanical ventilation.
Discussion: The case presented reflects importance of thiamine repletion in patients with hepatic encephalopathy. Thiamine deficiency is common in many forms of cirrhosis particularly alcoholic liver disease where it is caused by inadequate dietary intake, decreased hepatic storage, and impairment of intestinal thiamine absorption by ethanol. Wernicke's encephalopathy is a seriously under-diagnosed metabolic encephalopathy with severe neurological symptoms and region-selective neuronal cell death caused by thiamine deficiency is often encountered in chronic alcoholism. Thiamine supplementation must be added on early in patients with end stage liver disease especially in critical illnesses.
Disclosures:
Anumeet S. Tuli, MD, MBBS1, Mohammad Alqaisieh, MD1, Ahmad Alayyat, MD1, Sergio Quijano, MD2, Paige House, NP1. P1414 - Thiamine Terminated Mechanical Ventilation in Hepatic Encephalopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Hamilton Medical Center, Dalton, GA; 2Hamilton Health Care System, Dalton, GA
Introduction: Thiamine deficiency is common in chronic liver failure, which also causes increased brain ammonia concentrations. Both ammonia and thiamine deficiency result in decreased activity of alpha-ketoglutarate dehydrogenase resulting in a mitochondrial oxidative deficit in brain and consequent increases in brain lactate, oxidative stress, cellular energy impairment and release of pro-inflammatory cytokines.
Case Description/Methods: 50-year-old male with PMHx of alcoholic liver cirrhosis, chronic anemia, type 2 diabetes mellitus, alcohol abuse and gastric ulcer presented with chief complaints of nausea, vomiting and diarrhea of 10 days duration associated with inability of tolerating oral intake. Last alcohol use 2 weeks ago. Vitals stable on room air, alert and oriented to time, place, person and situation.
IV fluids and broad-spectrum antibiotics were started to treat acute kidney injury and suspected sepsis, given the markedly elevated WBC of 25000/mcL and lactic acid of 5.1 mmol/L. Ultrasound guided paracentesis aspirated 5L of clear fluid of transudative nature with no evidence of SBP.
On the second day of admission, patient noted to have tachycardia with GCS of 3. This prompted intubation and transfer to ICU. Work up including CT head, blood cultures, echocardiogram, C3, C4, hepatitis panel, smooth muscle antibody, HIV, Treponema pallidum, Vitamin B12, folate, TSH, lipase returned unremarkable. Ammonia level was 131, and the patient was started on lactulose enemas along with Rifaximin, without improvement for two days. Patient was then started on high dose of thiamine. Thiamine levels collected prior to replenishment demonstrated thiamine deficiency (Image 1). Three days after high dose thiamine supplementation, patient was noted to be alert and oriented leading to discontinuation of mechanical ventilation.
Discussion: The case presented reflects importance of thiamine repletion in patients with hepatic encephalopathy. Thiamine deficiency is common in many forms of cirrhosis particularly alcoholic liver disease where it is caused by inadequate dietary intake, decreased hepatic storage, and impairment of intestinal thiamine absorption by ethanol. Wernicke's encephalopathy is a seriously under-diagnosed metabolic encephalopathy with severe neurological symptoms and region-selective neuronal cell death caused by thiamine deficiency is often encountered in chronic alcoholism. Thiamine supplementation must be added on early in patients with end stage liver disease especially in critical illnesses.
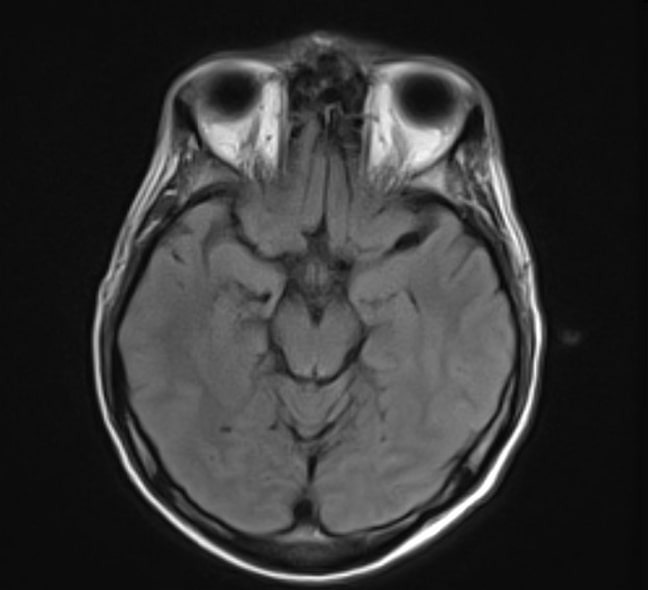
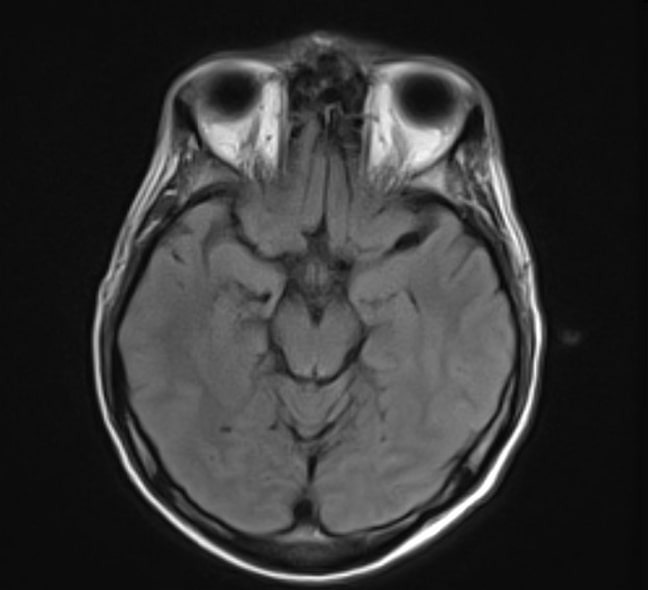
Figure: MRI brain- Subtle FLAIR hyperintensity surrounding periaqueductal gray matter which can be seen in setting of Wernicke’s encephalopathy.
Disclosures:
Anumeet Tuli indicated no relevant financial relationships.
Mohammad Alqaisieh indicated no relevant financial relationships.
Ahmad Alayyat indicated no relevant financial relationships.
Sergio Quijano indicated no relevant financial relationships.
Paige House indicated no relevant financial relationships.
Anumeet S. Tuli, MD, MBBS1, Mohammad Alqaisieh, MD1, Ahmad Alayyat, MD1, Sergio Quijano, MD2, Paige House, NP1. P1414 - Thiamine Terminated Mechanical Ventilation in Hepatic Encephalopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
