Sunday Poster Session
Category: Liver
P1418 - Drug-Induced Autoimmune-Like Hepatitis Secondary to Atorvastatin: A Diagnostic Dilemma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Heffernan, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Michael Heffernan, MD, Saim Ajmal, , Sheila Eswaran, MD, MS
Rush University Medical Center, Chicago, IL
Introduction: Drug-induced autoimmune-like hepatitis (DI-ALH) is an increasingly recognized phenotype of drug-induced liver injury (DILI). It can present a challenging diagnosis in patients with elevated LFTs and is important to consider for treatment strategies. This represents a case of a patient with suspected DI-ALH.
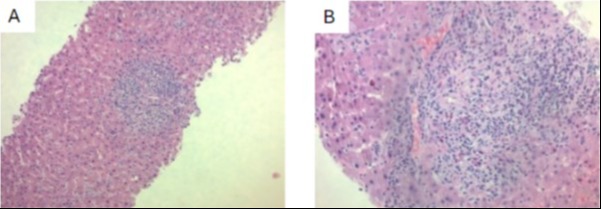
Case Description/Methods: An 85-year-old female with a history of atrial fibrillation, hypertension, and prior stroke was started on atorvastatin for secondary stroke prevention. 4 months later she developed fatigue, fevers, unintentional weight loss, acholic stools, and dark urine. Physical examination revealed jaundice but was otherwise unremarkable. Serologic evaluation revealed newly elevated ALT 178 U/L, AST 256 U/L, total bilirubin 3.9 mg/dL, INR 1.10. Her infectious hepatitis (A, B, C) studies were negative. Abdominal ultrasonography showed mildly increased echogenicity of liver parenchyma and no evidence of biliary abnormalities. Computed tomography (CT) of the abdomen/pelvis was unremarkable. Further laboratory evaluation showed a negative ANA, AMA, HIV, and Quant gold. However, it revealed a positive ASMA to 38, elevated IgM to 317 (normal IgG and IgA), positive monospot, positive CMV IgG and IgM, positive EBV IgG, and negative EBV IgM. Her TTE showed a normal EF. She underwent MRCP showing mild intrahepatic biliary dilatation and ERCP without biliary pathology. A liver biopsy showed grade 3 hepatitis with portal inflammation, increased plasma cells, and cholangitis with inflammatory destruction of bile ducts and numerous eosinophils. EBV and CMV stains were negative, so felt the serologies were falsely positive. These histologic features were concerning for DILI and/or AIH. The patient was diagnosed with drug-induced autoimmune-like hepatitis, her atorvastatin was discontinued, and she was started on prednisone 40mg daily. After starting prednisone, the patient had improvement in her LFTs and 1 month later they had normalized.
Discussion: DI-ALH hepatitis remains a diagnosis not well defined in the literature. In our patient, the diagnosis was initially unclear given the recent initiation of atorvastatin along with the elevated ASMA and histology consistent with both DILI and AIH. High clinical suspicion allows an earlier diagnosis to begin initiation of treatment. This case represents a positive clinical outcome and response to treatment, however, further characterization of the DI-ALH phenotype is required to standardize treatment regimens to improve morbidity in this cohort.
Disclosures:
Michael Heffernan, MD, Saim Ajmal, , Sheila Eswaran, MD, MS. P1418 - Drug-Induced Autoimmune-Like Hepatitis Secondary to Atorvastatin: A Diagnostic Dilemma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Drug-induced autoimmune-like hepatitis (DI-ALH) is an increasingly recognized phenotype of drug-induced liver injury (DILI). It can present a challenging diagnosis in patients with elevated LFTs and is important to consider for treatment strategies. This represents a case of a patient with suspected DI-ALH.
Case Description/Methods: An 85-year-old female with a history of atrial fibrillation, hypertension, and prior stroke was started on atorvastatin for secondary stroke prevention. 4 months later she developed fatigue, fevers, unintentional weight loss, acholic stools, and dark urine. Physical examination revealed jaundice but was otherwise unremarkable. Serologic evaluation revealed newly elevated ALT 178 U/L, AST 256 U/L, total bilirubin 3.9 mg/dL, INR 1.10. Her infectious hepatitis (A, B, C) studies were negative. Abdominal ultrasonography showed mildly increased echogenicity of liver parenchyma and no evidence of biliary abnormalities. Computed tomography (CT) of the abdomen/pelvis was unremarkable. Further laboratory evaluation showed a negative ANA, AMA, HIV, and Quant gold. However, it revealed a positive ASMA to 38, elevated IgM to 317 (normal IgG and IgA), positive monospot, positive CMV IgG and IgM, positive EBV IgG, and negative EBV IgM. Her TTE showed a normal EF. She underwent MRCP showing mild intrahepatic biliary dilatation and ERCP without biliary pathology. A liver biopsy showed grade 3 hepatitis with portal inflammation, increased plasma cells, and cholangitis with inflammatory destruction of bile ducts and numerous eosinophils. EBV and CMV stains were negative, so felt the serologies were falsely positive. These histologic features were concerning for DILI and/or AIH. The patient was diagnosed with drug-induced autoimmune-like hepatitis, her atorvastatin was discontinued, and she was started on prednisone 40mg daily. After starting prednisone, the patient had improvement in her LFTs and 1 month later they had normalized.
Discussion: DI-ALH hepatitis remains a diagnosis not well defined in the literature. In our patient, the diagnosis was initially unclear given the recent initiation of atorvastatin along with the elevated ASMA and histology consistent with both DILI and AIH. High clinical suspicion allows an earlier diagnosis to begin initiation of treatment. This case represents a positive clinical outcome and response to treatment, however, further characterization of the DI-ALH phenotype is required to standardize treatment regimens to improve morbidity in this cohort.
Figure: Figure 1. (A) Liver biopsy showing portal inflammation with presence of eosinophils and plasma cells. (B) Higher resolution image.
Disclosures:
Michael Heffernan indicated no relevant financial relationships.
Saim Ajmal indicated no relevant financial relationships.
Sheila Eswaran indicated no relevant financial relationships.
Michael Heffernan, MD, Saim Ajmal, , Sheila Eswaran, MD, MS. P1418 - Drug-Induced Autoimmune-Like Hepatitis Secondary to Atorvastatin: A Diagnostic Dilemma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
