Sunday Poster Session
Category: Obesity
P1456 - Semaglutide’s Hidden Perils: A Rare Case of Malnutrition and Wernicke Encephalopathy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suhaib Alhaj Ali, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Suhib Alhaj Ali, MD1, Majd Khadra, MD2, Mina Sitto, BS1, Madison Graifman, BS1, John Gietzen, MD1
1Henry Ford Hospital, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI
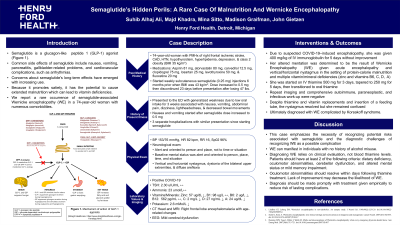
Introduction: With increasing use, concerns about semaglutide's long-term effects have been raised due to its potential to cause extended malnutrition, which can lead to vitamin deficiencies such as thiamine even without a history of alcohol use. We report a rare case of semaglutide-associated Wernicke Encephalopathy (WE) in an older adult with numerous comorbidities.
Case Description/Methods: A 74-year-old woman with history of ischemic stroke, coronary artery disease, hypertension, hypothyroidism, depression, & class 2 obesity (BMI 35 kg/m²) presented to the emergency department with generalized weakness after 3 days of low oral intake & decreased appetite. She was adherent to her medications, including semaglutide initiated 6 months & subsequently stopped 2 months prior (following 47 lbs weight loss) due to nausea, vomiting, abdominal pain, fatigue, lightheadedness, generalized weakness, & decreased bowel movements with the 0.5 mg dose, resulting in three hospitalizations. She exhibited changes in mental status, oriented to person & place but not to time or situation. Notable findings included incidental COVID-19 infection, vertical & horizontal nystagmus, & diffuse areflexia. Diagnostic imaging revealed right frontal lobe encephalomalacia & chronic micro-idiopathic alterations, while EEG indicated mild cerebral dysfunction. Thyroid stimulating hormone, vitamin B12, ammonia, & infectious/paraneoplastic/autoimmune workup were negative. She was treated with IV immunoglobulin for possible COVID-19-induced encephalopathy without improvement. Ultimately, her symptoms were attributed to WE & axonal neuropathy due to protein-calorie malnutrition & multiple vitamin/mineral deficiencies (zinc & vitamins B6, C, D, A). Treatment with IV thiamine was empirically initiated & continued despite a normal serum thiamine level, but her cognitive condition remained poor, leading to a diagnosis of WE possibly complicated by Korsakoff syndrome. She was ultimately discharged to hospice care.
Discussion: This case underscores the need for awareness of the risks associated with semaglutide, along with the diagnostic challenges in recognizing WE as a complication of semaglutide-induced nutritional deficiency. While traditionally linked to alcohol use, WE should be considered when patients present with prolonged dietary deficiencies, altered mental status, & oculomotor abnormalities even in the setting of normal serum thiamine. Diagnosis should be made promptly & treatment given empirically to reduce risk of lasting complications.
Disclosures:
Suhib Alhaj Ali, MD1, Majd Khadra, MD2, Mina Sitto, BS1, Madison Graifman, BS1, John Gietzen, MD1. P1456 - Semaglutide’s Hidden Perils: A Rare Case of Malnutrition and Wernicke Encephalopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: With increasing use, concerns about semaglutide's long-term effects have been raised due to its potential to cause extended malnutrition, which can lead to vitamin deficiencies such as thiamine even without a history of alcohol use. We report a rare case of semaglutide-associated Wernicke Encephalopathy (WE) in an older adult with numerous comorbidities.
Case Description/Methods: A 74-year-old woman with history of ischemic stroke, coronary artery disease, hypertension, hypothyroidism, depression, & class 2 obesity (BMI 35 kg/m²) presented to the emergency department with generalized weakness after 3 days of low oral intake & decreased appetite. She was adherent to her medications, including semaglutide initiated 6 months & subsequently stopped 2 months prior (following 47 lbs weight loss) due to nausea, vomiting, abdominal pain, fatigue, lightheadedness, generalized weakness, & decreased bowel movements with the 0.5 mg dose, resulting in three hospitalizations. She exhibited changes in mental status, oriented to person & place but not to time or situation. Notable findings included incidental COVID-19 infection, vertical & horizontal nystagmus, & diffuse areflexia. Diagnostic imaging revealed right frontal lobe encephalomalacia & chronic micro-idiopathic alterations, while EEG indicated mild cerebral dysfunction. Thyroid stimulating hormone, vitamin B12, ammonia, & infectious/paraneoplastic/autoimmune workup were negative. She was treated with IV immunoglobulin for possible COVID-19-induced encephalopathy without improvement. Ultimately, her symptoms were attributed to WE & axonal neuropathy due to protein-calorie malnutrition & multiple vitamin/mineral deficiencies (zinc & vitamins B6, C, D, A). Treatment with IV thiamine was empirically initiated & continued despite a normal serum thiamine level, but her cognitive condition remained poor, leading to a diagnosis of WE possibly complicated by Korsakoff syndrome. She was ultimately discharged to hospice care.
Discussion: This case underscores the need for awareness of the risks associated with semaglutide, along with the diagnostic challenges in recognizing WE as a complication of semaglutide-induced nutritional deficiency. While traditionally linked to alcohol use, WE should be considered when patients present with prolonged dietary deficiencies, altered mental status, & oculomotor abnormalities even in the setting of normal serum thiamine. Diagnosis should be made promptly & treatment given empirically to reduce risk of lasting complications.
Disclosures:
Suhib Alhaj Ali indicated no relevant financial relationships.
Majd Khadra indicated no relevant financial relationships.
Mina Sitto indicated no relevant financial relationships.
Madison Graifman indicated no relevant financial relationships.
John Gietzen indicated no relevant financial relationships.
Suhib Alhaj Ali, MD1, Majd Khadra, MD2, Mina Sitto, BS1, Madison Graifman, BS1, John Gietzen, MD1. P1456 - Semaglutide’s Hidden Perils: A Rare Case of Malnutrition and Wernicke Encephalopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
