Sunday Poster Session
Category: Pediatrics
P1464 - Prenatal Exposure to Air Pollution and the Incidence of Pediatric Biliary Atresia: A Nationwide Longitudinal Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Shu-Yen Emily Chan, MD, MSc
Weiss Memorial Hospital
Chicago, IL
Presenting Author(s)
Emily Shu-Yen Chan, MD, MSc1, Meng-Che Wu, MD2, Noppachai Siranart, MD3, Chieh-Chung Lin, MD4
1Weiss Memorial Hospital, Chicago, IL; 2Massachusetts General Hospital, Boston, IL; 3Brigham and Women's Hospital, Boston, MA; 4Taichung Veterans General Hospital, Taichung, Taichung, Taiwan
Introduction: Biliary atresia (BA) is a severe liver disease and the leading indication for liver transplantation in pediatric populations, though its etiology remains unclear. Previous studies suggested air pollution may cause oxidative stress and genotoxic effects, contributing to leukemia and Kawasaki disease in early childhood. This study aims to investigate the link between prenatal air pollution exposure and newborn BA risk.
Methods: This nationwide, longitudinal, matched case-control cohort study used electronic health records from the National Health Insurance Research Database (NHIRD) from 1/2004 to 12/2016. The NHIRD was linked with the Taiwan Maternal and Child Health Database to establish connections between mothers and their children. BA cases were identified in children under six using ICD-9-CM code: 751.61/ ICD-10-CM code: Q44.2 and who underwent the Kasai procedure or liver transplantation. Controls, matched by age, index month, and gender, were selected at a 1:10 ratio. Multivariable logistic regression models, adjusted for potential confounders (gestation age, maternal age, delivery mode, and birth weight), were utilized to assess the association between the Pollutant Standards Index (PSI) and individual air pollutants (SO₂, CO, O₃, PM₂.₅, PM₁₀, NO, NO₂, and NOx) and BA development. Quartiles of cumulative air pollutant amounts were also analyzed for dose-dependent effects.
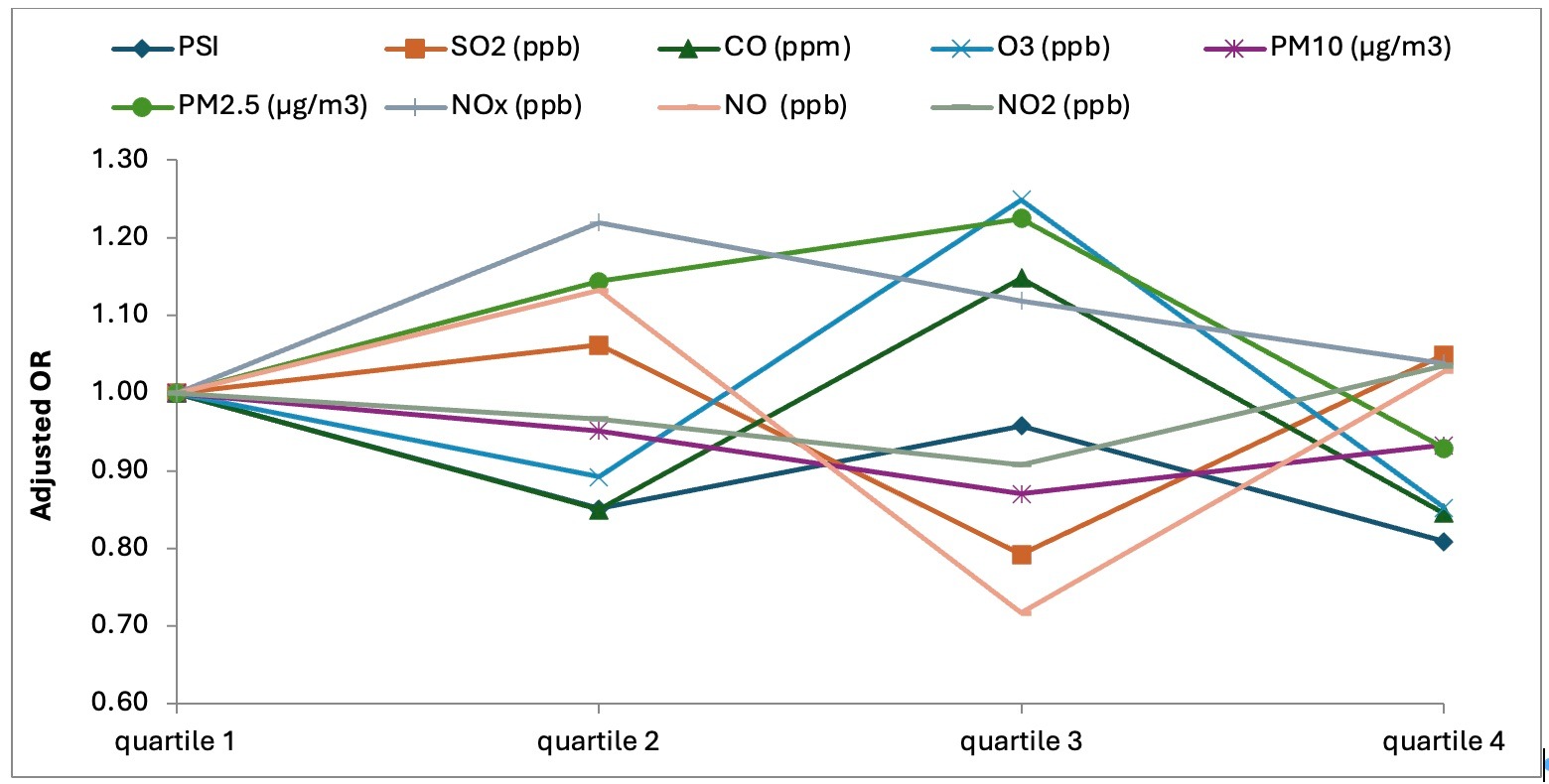
Results: A total of 1,662,727 first-time pregnancies were identified from 2004 to 2016. After excluding 8,527 newborns due to congenital neonatal defects, 1,654,200 individuals remained. Among them, a cohort of 253 BA patients was identified. After adjusting for multiple confounders, no significant associations were found between prenatal air pollution exposure and BA risk. However, infants weighing less than 2500g at birth had a significantly higher BA risk compared to those weighing 2500g or more (aOR: 1.92, 95% CI: 1.25-3.01, p=0.003). No significant differences were noticed in gender, maternal age, delivery mode, gestational age, or maternal comorbidities (asthma, allergic rhinitis, atopic dermatitis) between the two groups. Quartile analysis of cumulative air pollutant exposure also indicated no dose-response relationship with BA risk for air pollutants.
Discussion: In this population-based study conducted in Taiwan, no significant correlation was found between prenatal exposure to air pollutions and the risk of newborn BA.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Shu-Yen Chan, MD, MSc1, Meng-Che Wu, MD2, Noppachai Siranart, MD3, Chieh-Chung Lin, MD4. P1464 - Prenatal Exposure to Air Pollution and the Incidence of Pediatric Biliary Atresia: A Nationwide Longitudinal Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Weiss Memorial Hospital, Chicago, IL; 2Massachusetts General Hospital, Boston, IL; 3Brigham and Women's Hospital, Boston, MA; 4Taichung Veterans General Hospital, Taichung, Taichung, Taiwan
Introduction: Biliary atresia (BA) is a severe liver disease and the leading indication for liver transplantation in pediatric populations, though its etiology remains unclear. Previous studies suggested air pollution may cause oxidative stress and genotoxic effects, contributing to leukemia and Kawasaki disease in early childhood. This study aims to investigate the link between prenatal air pollution exposure and newborn BA risk.
Methods: This nationwide, longitudinal, matched case-control cohort study used electronic health records from the National Health Insurance Research Database (NHIRD) from 1/2004 to 12/2016. The NHIRD was linked with the Taiwan Maternal and Child Health Database to establish connections between mothers and their children. BA cases were identified in children under six using ICD-9-CM code: 751.61/ ICD-10-CM code: Q44.2 and who underwent the Kasai procedure or liver transplantation. Controls, matched by age, index month, and gender, were selected at a 1:10 ratio. Multivariable logistic regression models, adjusted for potential confounders (gestation age, maternal age, delivery mode, and birth weight), were utilized to assess the association between the Pollutant Standards Index (PSI) and individual air pollutants (SO₂, CO, O₃, PM₂.₅, PM₁₀, NO, NO₂, and NOx) and BA development. Quartiles of cumulative air pollutant amounts were also analyzed for dose-dependent effects.
Results: A total of 1,662,727 first-time pregnancies were identified from 2004 to 2016. After excluding 8,527 newborns due to congenital neonatal defects, 1,654,200 individuals remained. Among them, a cohort of 253 BA patients was identified. After adjusting for multiple confounders, no significant associations were found between prenatal air pollution exposure and BA risk. However, infants weighing less than 2500g at birth had a significantly higher BA risk compared to those weighing 2500g or more (aOR: 1.92, 95% CI: 1.25-3.01, p=0.003). No significant differences were noticed in gender, maternal age, delivery mode, gestational age, or maternal comorbidities (asthma, allergic rhinitis, atopic dermatitis) between the two groups. Quartile analysis of cumulative air pollutant exposure also indicated no dose-response relationship with BA risk for air pollutants.
Discussion: In this population-based study conducted in Taiwan, no significant correlation was found between prenatal exposure to air pollutions and the risk of newborn BA.
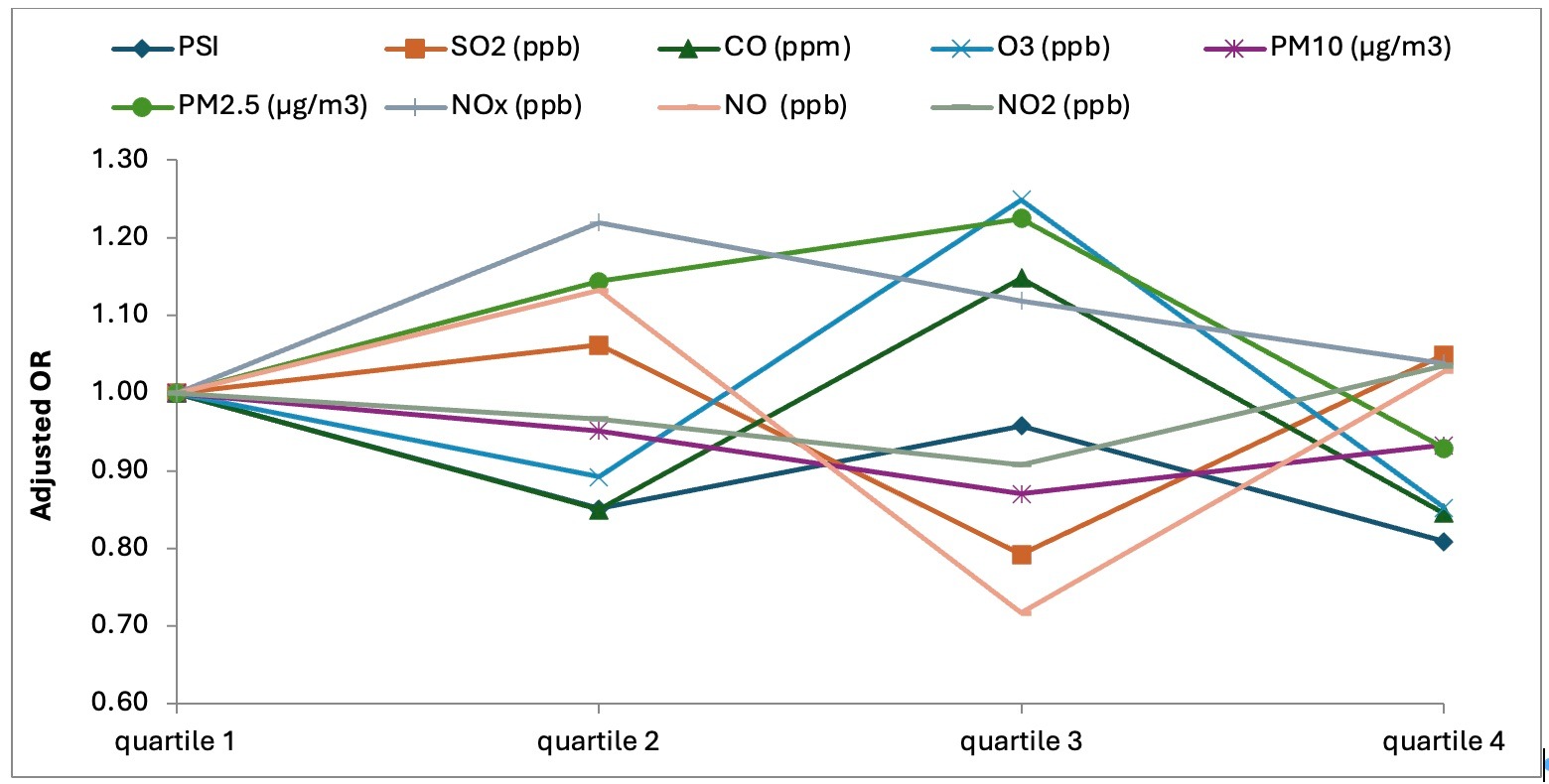
Figure: Figure 2. Quartiles of prenatal cumulative air pollutant exposure to the risk of pediatric biliary atresia
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Meng-Che Wu indicated no relevant financial relationships.
Noppachai Siranart indicated no relevant financial relationships.
Chieh-Chung Lin indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD, MSc1, Meng-Che Wu, MD2, Noppachai Siranart, MD3, Chieh-Chung Lin, MD4. P1464 - Prenatal Exposure to Air Pollution and the Incidence of Pediatric Biliary Atresia: A Nationwide Longitudinal Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
