Sunday Poster Session
Category: Pediatrics
P1475 - Pancreatic Solid Pseudopapillary Neoplasm in an Adolescent Demonstrating Rare Spontaneous Regression
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SM
Sukrita S. Mysore, MBBS
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Sukrita S. Mysore, MBBS1, Howard Kader, MD2
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Pancreatic tumors have an annual incidence of 0.19 cases per million in the pediatric population in North America. Solid pseudopapillary neoplasms (SPN), an indolent tumor with low malignant potential, comprise 70% of pediatric pancreatic tumors. It has been described mostly in adolescents, mean age of 13-14 years. SPN commonly occurs in the pancreatic tail with surgery being the mainstay of treatment. We present a case of a 13-year-old female who presented with acute onset abdominal pain found to have SPN based on endoscopic ultrasound assisted biopsy with spontaneous regression of the mass.
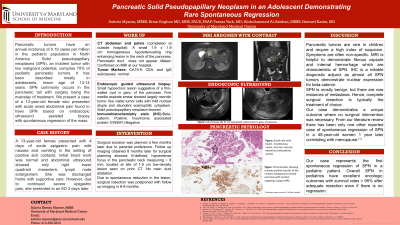
Case Description/Methods: A 13-year-old female presented with 4 days of acute epigastric pain with nausea and vomiting in the setting of positive sick contacts. Initial blood work was normal and abdominal ultrasound showed only right lower quadrant mesenteric lymph node enlargement. She was discharged home with supportive care. However, due to continued severe epigastric pain, she presented to an ED 2 days later. CT scan of the abdomen & pelvis showed a small homogeneous hypoattenuating ring enhancing lesion in the neck of the pancreas which was confirmed by MRI upon transfer. The CA19-9, CEA, and IgG subclasses were normal. Endoscopic guided ultrasound biopsy showed a small hypoechoic lesion suggestive of a thin-walled cyst in the genu of the pancreas with pathology favoring a solid pseudopapillary neoplasm as the cause of the lesion with nuclear immunostaining (IHC) being positive for Beta-catenin and negative for INSM1. Surgical excision was planned, however follow up imaging 8 months later showed only a subtle focus of abnormal signal in the pancreatic neck. Due to spontaneous reduction in the lesion, surgical resection was postponed with follow up imaging in 6-8 months.
Discussion: Pancreatic tumors are rare in children and require a high index of suspicion. SPN rarely metastasizes. Symptoms are often non-specific. IHC is a reliable diagnostic adjunct as almost all SPN tumors demonstrate nuclear expression for beta-catenin. MRI is helpful to demonstrate fibrous capsule and internal hemorrhage which are characteristic of SPN. Complete surgical resection is typically the treatment of choice. Our case demonstrates a unique outcome where no surgical intervention was necessary. Overall SPN in pediatrics have excellent oncologic outcomes with survival rates > 95% after adequate resection.
Disclosures:
Sukrita S. Mysore, MBBS1, Howard Kader, MD2. P1475 - Pancreatic Solid Pseudopapillary Neoplasm in an Adolescent Demonstrating Rare Spontaneous Regression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Pancreatic tumors have an annual incidence of 0.19 cases per million in the pediatric population in North America. Solid pseudopapillary neoplasms (SPN), an indolent tumor with low malignant potential, comprise 70% of pediatric pancreatic tumors. It has been described mostly in adolescents, mean age of 13-14 years. SPN commonly occurs in the pancreatic tail with surgery being the mainstay of treatment. We present a case of a 13-year-old female who presented with acute onset abdominal pain found to have SPN based on endoscopic ultrasound assisted biopsy with spontaneous regression of the mass.
Case Description/Methods: A 13-year-old female presented with 4 days of acute epigastric pain with nausea and vomiting in the setting of positive sick contacts. Initial blood work was normal and abdominal ultrasound showed only right lower quadrant mesenteric lymph node enlargement. She was discharged home with supportive care. However, due to continued severe epigastric pain, she presented to an ED 2 days later. CT scan of the abdomen & pelvis showed a small homogeneous hypoattenuating ring enhancing lesion in the neck of the pancreas which was confirmed by MRI upon transfer. The CA19-9, CEA, and IgG subclasses were normal. Endoscopic guided ultrasound biopsy showed a small hypoechoic lesion suggestive of a thin-walled cyst in the genu of the pancreas with pathology favoring a solid pseudopapillary neoplasm as the cause of the lesion with nuclear immunostaining (IHC) being positive for Beta-catenin and negative for INSM1. Surgical excision was planned, however follow up imaging 8 months later showed only a subtle focus of abnormal signal in the pancreatic neck. Due to spontaneous reduction in the lesion, surgical resection was postponed with follow up imaging in 6-8 months.
Discussion: Pancreatic tumors are rare in children and require a high index of suspicion. SPN rarely metastasizes. Symptoms are often non-specific. IHC is a reliable diagnostic adjunct as almost all SPN tumors demonstrate nuclear expression for beta-catenin. MRI is helpful to demonstrate fibrous capsule and internal hemorrhage which are characteristic of SPN. Complete surgical resection is typically the treatment of choice. Our case demonstrates a unique outcome where no surgical intervention was necessary. Overall SPN in pediatrics have excellent oncologic outcomes with survival rates > 95% after adequate resection.
Disclosures:
Sukrita Mysore indicated no relevant financial relationships.
Howard Kader indicated no relevant financial relationships.
Sukrita S. Mysore, MBBS1, Howard Kader, MD2. P1475 - Pancreatic Solid Pseudopapillary Neoplasm in an Adolescent Demonstrating Rare Spontaneous Regression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
