Sunday Poster Session
Category: Pediatrics
P1483 - CODE Brown: A Case of a Novel Variant of a DGAT1 Mutation Causing DIAR7
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Samantha Pendleton, DO
University of Massachusetts Chan Medical School - Baystate Medical Center
Springfield, MA
Presenting Author(s)
Samantha Pendleton, DO1, Mojdeh Mostafavi, MD2, Timothy Menz, MD3, Wael Sayej, MD3
1University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 2Massachusetts General Hospital, Harvard Medical School, Boston, MA; 3Baystate Medical Center, Springfield, MA
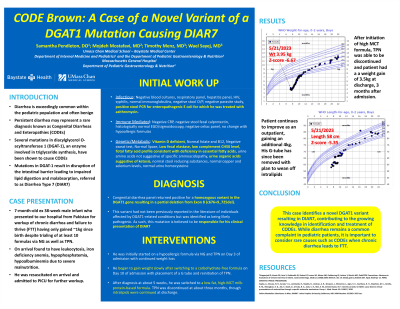
Introduction: While occasional diarrhea is exceedingly common within the pediatric population and often benign, persistent diarrhea is more frequently pathologic in nature and may represent a rare diagnosis known as Congenital Diarrheas and Enteropathies (CODEs). Several mutations in diacylglycerol O-acyltransferase 1 (DGAT-1), an enzyme involved in triglyceride synthesis, have been shown to cause CODEs. It is hypothesized that such mutations in DGAT-1 result in disruption of the intestinal barrier leading to impaired lipid digestion and malabsorption, referred to as Diarrhea Type 7 (DIAR7).
Case Description/Methods: We present a case of an initially 7-month-old male infant who presented to our hospital from Pakistan for workup of chronic diarrhea and failure to thrive (FTT). He had gained only ~1kg since birth despite trialing of several formulas via NG as well as total parenteral nutrition. Upon arrival to our hospital, he required resuscitation in the pediatric ICU and underwent a largely negative workup including normal stool reducing substances, fecal calprotectin, negative stool ova/parasite, and a grossly and histologically normal EGD/sigmoidoscopy. His fecal elastase was low, and PCR did return positive for enteropathogenic E. coli, for which he received a 3-day course of azithromycin. He began to gain weight slowly after switching to a carbohydrate-free formula with placement of a G tube and reinitiation of TPN. Five weeks into admission the congenital diarrhea panel returned positive with a homozygous variant in the DGAT1 gene resulting in a partial deletion from Exon 8 (c676+9_725del). This variant had not been previously reported in the literature of individuals affected by DGAT1-related conditions but was identified as being likely pathogenic. As such, this mutation is believed to be responsible for his clinical presentation of DIAR7. He was switched to a low-fat, high-MCT milk-protein-based formula and continued intralipids with a weight gain of 3.5kg at discharge, 3 months after admission. Patient continued to improve as an outpatient, gaining an additional 4kg. His G-tube has since been removed with plan to wean off intralipids.
Discussion: This case identifies a novel DGAT1 variant resulting in DIAR7, contributing to the growing knowledge in identification and treatment of CODEs. While diarrhea remains a common complaint in pediatric patients, it is important to consider rare causes such as CODEs when chronic diarrhea leads to FTT.
Disclosures:
Samantha Pendleton, DO1, Mojdeh Mostafavi, MD2, Timothy Menz, MD3, Wael Sayej, MD3. P1483 - CODE Brown: A Case of a Novel Variant of a DGAT1 Mutation Causing DIAR7, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 2Massachusetts General Hospital, Harvard Medical School, Boston, MA; 3Baystate Medical Center, Springfield, MA
Introduction: While occasional diarrhea is exceedingly common within the pediatric population and often benign, persistent diarrhea is more frequently pathologic in nature and may represent a rare diagnosis known as Congenital Diarrheas and Enteropathies (CODEs). Several mutations in diacylglycerol O-acyltransferase 1 (DGAT-1), an enzyme involved in triglyceride synthesis, have been shown to cause CODEs. It is hypothesized that such mutations in DGAT-1 result in disruption of the intestinal barrier leading to impaired lipid digestion and malabsorption, referred to as Diarrhea Type 7 (DIAR7).
Case Description/Methods: We present a case of an initially 7-month-old male infant who presented to our hospital from Pakistan for workup of chronic diarrhea and failure to thrive (FTT). He had gained only ~1kg since birth despite trialing of several formulas via NG as well as total parenteral nutrition. Upon arrival to our hospital, he required resuscitation in the pediatric ICU and underwent a largely negative workup including normal stool reducing substances, fecal calprotectin, negative stool ova/parasite, and a grossly and histologically normal EGD/sigmoidoscopy. His fecal elastase was low, and PCR did return positive for enteropathogenic E. coli, for which he received a 3-day course of azithromycin. He began to gain weight slowly after switching to a carbohydrate-free formula with placement of a G tube and reinitiation of TPN. Five weeks into admission the congenital diarrhea panel returned positive with a homozygous variant in the DGAT1 gene resulting in a partial deletion from Exon 8 (c676+9_725del). This variant had not been previously reported in the literature of individuals affected by DGAT1-related conditions but was identified as being likely pathogenic. As such, this mutation is believed to be responsible for his clinical presentation of DIAR7. He was switched to a low-fat, high-MCT milk-protein-based formula and continued intralipids with a weight gain of 3.5kg at discharge, 3 months after admission. Patient continued to improve as an outpatient, gaining an additional 4kg. His G-tube has since been removed with plan to wean off intralipids.
Discussion: This case identifies a novel DGAT1 variant resulting in DIAR7, contributing to the growing knowledge in identification and treatment of CODEs. While diarrhea remains a common complaint in pediatric patients, it is important to consider rare causes such as CODEs when chronic diarrhea leads to FTT.
Disclosures:
Samantha Pendleton indicated no relevant financial relationships.
Mojdeh Mostafavi indicated no relevant financial relationships.
Timothy Menz indicated no relevant financial relationships.
Wael Sayej indicated no relevant financial relationships.
Samantha Pendleton, DO1, Mojdeh Mostafavi, MD2, Timothy Menz, MD3, Wael Sayej, MD3. P1483 - CODE Brown: A Case of a Novel Variant of a DGAT1 Mutation Causing DIAR7, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

