Sunday Poster Session
Category: Small Intestine
P1555 - Complicated Duodenal Diverticulitis: A Case of Conservative Medical Management
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Iyad Al-Bustami, MD, MPH(c)
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Iyad Al-bustami, MD, MPH(c)1, Abid Qureshi, MD2, Shamsa M. Qaadri, BSc3, Shafiq Qaadri, BA4, Amogh R. Kare, BS3, Saira Shah, MD2, Saigopal R. Gujjula, MD2, Anuj R. Sharma, MBBS2, Kenan Alrejjal, MBBS5, Nitish Mittal, MD6, Kazi T. Haque, MD7, Shahzaib Ahmed, MBBS8, Vikash Kumar, MD9, Camelia Ciobanu, MD2, Amr Dokmak, MD2, Ali Wakil, MD2, Denzil Etienne, MD2, Madhavi Reddy, MD, FACG2
1Brooklyn Hospital Center, Houston, TX; 2Brooklyn Hospital Center, Brooklyn, NY; 3St. George's University School of Medicine, Brooklyn, NY; 4Toronto Metropolitan University, Toronto, ON, Canada; 5MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 6University of Texas Health, McGovern Medical School, Houston, TX; 7University of Texas Health, McGovern Medical School, Pearland, TX; 8Fatima Memorial Hospital College of Medicine and Dentistry, Lahore, Punjab, Pakistan; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: The duodenum is a common site for small bowel diverticula with only 1-5% being symptomatic. Diverticula rarely perforates causing a presentation of an acute abdomen. Here, we report a case of an immediate onset complication of a duodenal diverticulitis, with a contained perforation in the 4th part of the duodenum.
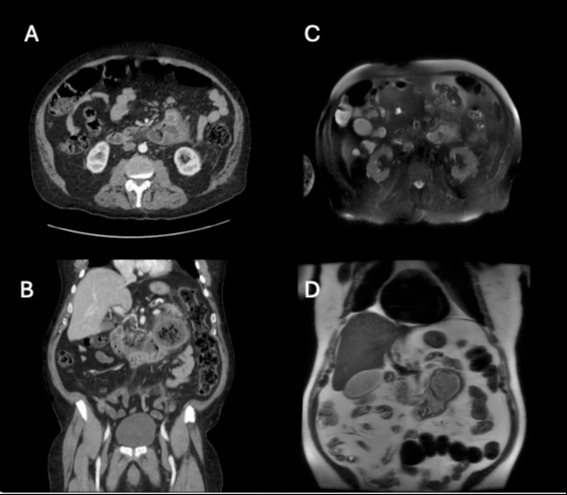
Case Description/Methods: A 71-year-old male with a past medical history of hypertension and diabetes mellitus presented to emergency with a one day history of vague abdominal pain and nausea. White blood count elevated to 18.6k with major left shift, normal amylase & lipase levels. CT abdominal and pelvis showed a complex large thick-walled collection measuring 7.1 x 6.6 x 8.0 cm, arising off the 4th portion of the duodenum with surrounding stranding/inflammation as well as peripancreatic stranding at the body and tail, concerning for complicated peripancreatic fluid collection sequelae of pancreatitis vs complicated diverticulitis vs contained perforation (fig.1). MRI abdomen and pelvis was performed to further characterization of the pancreatic parenchyma: redemonstrating duodenal diverticulitis with a small focal outpouching arising from the base of the diverticulum, while pancreatic parenchyma appeared as low to intermediate signal on T2-weighted images (fig.1). Due to difficult anatomy, there was no safe window for drainage, this patient successfully was managed conservatively with intravenous fluids & antibiotics; eventually managed to tolerate diet within 7 days.
Discussion: Symptomatic duodenal diverticulitis can be initially thought to be as a peripancreatic complicated fluid collection given anatomical proximity. In the setting of normal lipase & amylase levels, MRI can provide detailed characterization of the pancreas and organs’ structure. Different imaging modality can provide adequate accuracy to narrow differentials. Intra-abdominal source control of infection is the ideal modality of management; which can also include a conservative approach after adequate risk-benefit evaluation.
Disclosures:
Iyad Al-bustami, MD, MPH(c)1, Abid Qureshi, MD2, Shamsa M. Qaadri, BSc3, Shafiq Qaadri, BA4, Amogh R. Kare, BS3, Saira Shah, MD2, Saigopal R. Gujjula, MD2, Anuj R. Sharma, MBBS2, Kenan Alrejjal, MBBS5, Nitish Mittal, MD6, Kazi T. Haque, MD7, Shahzaib Ahmed, MBBS8, Vikash Kumar, MD9, Camelia Ciobanu, MD2, Amr Dokmak, MD2, Ali Wakil, MD2, Denzil Etienne, MD2, Madhavi Reddy, MD, FACG2. P1555 - Complicated Duodenal Diverticulitis: A Case of Conservative Medical Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brooklyn Hospital Center, Houston, TX; 2Brooklyn Hospital Center, Brooklyn, NY; 3St. George's University School of Medicine, Brooklyn, NY; 4Toronto Metropolitan University, Toronto, ON, Canada; 5MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 6University of Texas Health, McGovern Medical School, Houston, TX; 7University of Texas Health, McGovern Medical School, Pearland, TX; 8Fatima Memorial Hospital College of Medicine and Dentistry, Lahore, Punjab, Pakistan; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: The duodenum is a common site for small bowel diverticula with only 1-5% being symptomatic. Diverticula rarely perforates causing a presentation of an acute abdomen. Here, we report a case of an immediate onset complication of a duodenal diverticulitis, with a contained perforation in the 4th part of the duodenum.
Case Description/Methods: A 71-year-old male with a past medical history of hypertension and diabetes mellitus presented to emergency with a one day history of vague abdominal pain and nausea. White blood count elevated to 18.6k with major left shift, normal amylase & lipase levels. CT abdominal and pelvis showed a complex large thick-walled collection measuring 7.1 x 6.6 x 8.0 cm, arising off the 4th portion of the duodenum with surrounding stranding/inflammation as well as peripancreatic stranding at the body and tail, concerning for complicated peripancreatic fluid collection sequelae of pancreatitis vs complicated diverticulitis vs contained perforation (fig.1). MRI abdomen and pelvis was performed to further characterization of the pancreatic parenchyma: redemonstrating duodenal diverticulitis with a small focal outpouching arising from the base of the diverticulum, while pancreatic parenchyma appeared as low to intermediate signal on T2-weighted images (fig.1). Due to difficult anatomy, there was no safe window for drainage, this patient successfully was managed conservatively with intravenous fluids & antibiotics; eventually managed to tolerate diet within 7 days.
Discussion: Symptomatic duodenal diverticulitis can be initially thought to be as a peripancreatic complicated fluid collection given anatomical proximity. In the setting of normal lipase & amylase levels, MRI can provide detailed characterization of the pancreas and organs’ structure. Different imaging modality can provide adequate accuracy to narrow differentials. Intra-abdominal source control of infection is the ideal modality of management; which can also include a conservative approach after adequate risk-benefit evaluation.
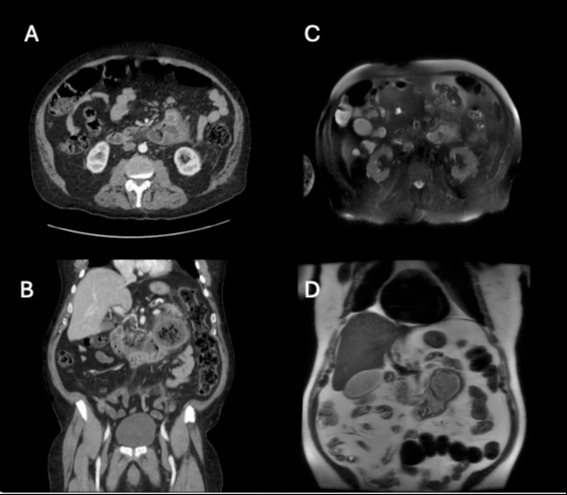
Figure: Fig1: A,B: CT Abdomen demonstrating complex lesion with fat stranding. C,D: MRI Abdomen demonstrating complicated duodenal diverticulitis.
Disclosures:
Iyad Al-bustami indicated no relevant financial relationships.
Abid Qureshi indicated no relevant financial relationships.
Shamsa Qaadri indicated no relevant financial relationships.
Shafiq Qaadri indicated no relevant financial relationships.
Amogh Kare indicated no relevant financial relationships.
Saira Shah indicated no relevant financial relationships.
Saigopal Gujjula indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Shahzaib Ahmed indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Iyad Al-bustami, MD, MPH(c)1, Abid Qureshi, MD2, Shamsa M. Qaadri, BSc3, Shafiq Qaadri, BA4, Amogh R. Kare, BS3, Saira Shah, MD2, Saigopal R. Gujjula, MD2, Anuj R. Sharma, MBBS2, Kenan Alrejjal, MBBS5, Nitish Mittal, MD6, Kazi T. Haque, MD7, Shahzaib Ahmed, MBBS8, Vikash Kumar, MD9, Camelia Ciobanu, MD2, Amr Dokmak, MD2, Ali Wakil, MD2, Denzil Etienne, MD2, Madhavi Reddy, MD, FACG2. P1555 - Complicated Duodenal Diverticulitis: A Case of Conservative Medical Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
