Sunday Poster Session
Category: Small Intestine
P1571 - A Case of Adult-Onset Henoch-Schonlein Purpura With Severe Jejunum Involvement
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Peter Senada, MD
University of Florida College of Medicine
Jacksonville, FL
Presenting Author(s)
Peter Senada, MD1, Mohammed Ahsan, MD2, Tara Kronen, DO, MA1, Lauren N.. Stemboroski, DO1
1University of Florida College of Medicine, Jacksonville, FL; 2NCH Healthcare System, Naples, FL
Introduction: Henoch-Schonlein purpura (HSP) is a small vessel vasculitis that affects multiple organ systems including the skin, kidneys and gastrointestinal (GI) system through a type III hypersensitivity reaction. While typically presenting in children, adult-onset HSP primarily manifests with renal involvement, with 85% having concurrent GI complaints including abdominal pain, diarrhea, vomiting, and bleeding. The most affected site is the descending segment of the duodenum, with cases also evident in the ileum and rectum. Our case demonstrates a unique presentation of adult-onset HSP presenting with GI manifestations at an atypical site, the jejunum
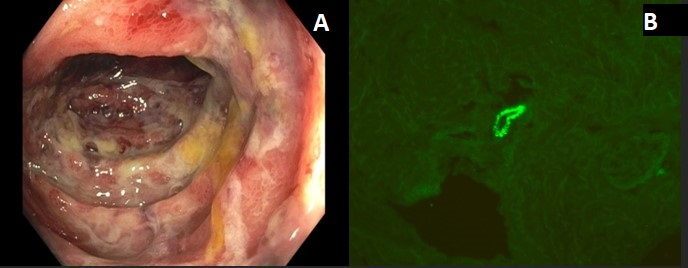
Case Description/Methods: A 21-year-old female presented with a 4-day history of severe epigastric abdominal pain, exacerbated with meals, and associated with new-onset diarrhea and nausea with non-bloody, non-bilious emesis. The patient denied melena, hematochezia, fever, chills, or a history of inflammatory bowel disease. She had a computed tomography (CT) abdomen/pelvis showing evidence of duodenitis and jejunitis, with mesenteric edema. Her labs were notable for leukocytosis of 17.9 x 109/L, creatinine 0.60 mg/dL, CRP of 103.4 mg/L and a urinalysis positive for hematuria. The patient had a negative infectious workup. Magnetic resonance enterography showed multisegmental jejunitis with intermittent stricturing and increased proximal jejunal distention. A small bowel enteroscopy was performed which showed a normal duodenum and a severely ulcerated jejunum. The patient did not improve with supportive care. 10 days after admission, the patient was found to have non-blanching petechiae of the ankles, upper thighs, and buttocks. Skin biopsy was performed of the petechial lesion. Findings showed a bullous leukocytoclastic vasculitis with weak IgA deposits in vessels. The patient was started on 40 mg IV methylprednisolone two times daily, followed by a 4-week prednisone taper, leading to the resolution of her symptoms
Discussion: The diagnosis of IgA vasculitis is made by at least two of the following criteria: palpable purpura, bowel angina, and biopsy with histological findings of IgA deposition. Our patient met all diagnostic criteria. An important clinical pearl in the workup of HSP is to first rule out infectious etiology, as treatment with corticosteroids can be life-threatening in the setting of an acute infection. Finally, it is important to keep IgA vasculitis on the differential in cases of jejunal ulcers, as HSP can be found throughout the small bowel
Disclosures:
Peter Senada, MD1, Mohammed Ahsan, MD2, Tara Kronen, DO, MA1, Lauren N.. Stemboroski, DO1. P1571 - A Case of Adult-Onset Henoch-Schonlein Purpura With Severe Jejunum Involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Jacksonville, FL; 2NCH Healthcare System, Naples, FL
Introduction: Henoch-Schonlein purpura (HSP) is a small vessel vasculitis that affects multiple organ systems including the skin, kidneys and gastrointestinal (GI) system through a type III hypersensitivity reaction. While typically presenting in children, adult-onset HSP primarily manifests with renal involvement, with 85% having concurrent GI complaints including abdominal pain, diarrhea, vomiting, and bleeding. The most affected site is the descending segment of the duodenum, with cases also evident in the ileum and rectum. Our case demonstrates a unique presentation of adult-onset HSP presenting with GI manifestations at an atypical site, the jejunum
Case Description/Methods: A 21-year-old female presented with a 4-day history of severe epigastric abdominal pain, exacerbated with meals, and associated with new-onset diarrhea and nausea with non-bloody, non-bilious emesis. The patient denied melena, hematochezia, fever, chills, or a history of inflammatory bowel disease. She had a computed tomography (CT) abdomen/pelvis showing evidence of duodenitis and jejunitis, with mesenteric edema. Her labs were notable for leukocytosis of 17.9 x 109/L, creatinine 0.60 mg/dL, CRP of 103.4 mg/L and a urinalysis positive for hematuria. The patient had a negative infectious workup. Magnetic resonance enterography showed multisegmental jejunitis with intermittent stricturing and increased proximal jejunal distention. A small bowel enteroscopy was performed which showed a normal duodenum and a severely ulcerated jejunum. The patient did not improve with supportive care. 10 days after admission, the patient was found to have non-blanching petechiae of the ankles, upper thighs, and buttocks. Skin biopsy was performed of the petechial lesion. Findings showed a bullous leukocytoclastic vasculitis with weak IgA deposits in vessels. The patient was started on 40 mg IV methylprednisolone two times daily, followed by a 4-week prednisone taper, leading to the resolution of her symptoms
Discussion: The diagnosis of IgA vasculitis is made by at least two of the following criteria: palpable purpura, bowel angina, and biopsy with histological findings of IgA deposition. Our patient met all diagnostic criteria. An important clinical pearl in the workup of HSP is to first rule out infectious etiology, as treatment with corticosteroids can be life-threatening in the setting of an acute infection. Finally, it is important to keep IgA vasculitis on the differential in cases of jejunal ulcers, as HSP can be found throughout the small bowel
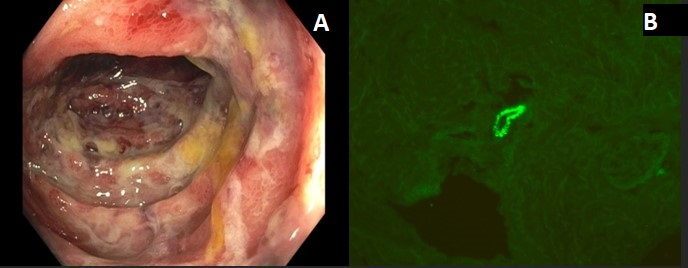
Figure: Figure 1: Small bowel enteroscopy with many non-bleeding deep jejunal ulcers that are friable, found 100 cm from incisors, without stigmata of bleeding.
Figure 2: Skin biopsy of purpura lesion on ankle. Immunofluorescence showed weak and patchy granular deposits in small and medium vessels. C3 showed strong deposits in medium sized vessels. Immunofluorescence studies for IgG, IgM, and fibrinogen were negative.
Figure 2: Skin biopsy of purpura lesion on ankle. Immunofluorescence showed weak and patchy granular deposits in small and medium vessels. C3 showed strong deposits in medium sized vessels. Immunofluorescence studies for IgG, IgM, and fibrinogen were negative.
Disclosures:
Peter Senada indicated no relevant financial relationships.
Mohammed Ahsan indicated no relevant financial relationships.
Tara Kronen indicated no relevant financial relationships.
Lauren Stemboroski indicated no relevant financial relationships.
Peter Senada, MD1, Mohammed Ahsan, MD2, Tara Kronen, DO, MA1, Lauren N.. Stemboroski, DO1. P1571 - A Case of Adult-Onset Henoch-Schonlein Purpura With Severe Jejunum Involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
