Sunday Poster Session
Category: Small Intestine
P1572 - Splenic infarct and SMA thrombosis as a manifestation of Seronegative Antiphospholipid Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sakshi Bai, MD,
Henry Ford Jackson Hospital
Jackson, MI
Presenting Author(s)
Sakshi Bai, MD,, Bipneet Singh, MD, Abraham Kisule, MD, Niroshan Ranjan, MD
Henry Ford Jackson Hospital, Jackson, MI
Introduction: Antiphospholipid Syndrome (APS) presents with a wide spectrum of clinical manifestations, ranging from asymptomatic cases to life-threatening catastrophic APS. Thrombosis in large or micro-vessels can affect virtually any organ system. Diagnostic criteria for APS have evolved, typically requiring the presence of one clinical criterion and one laboratory criterion. However, emerging research highlights cases where patients exhibit clinical features of APS despite transiently positive or persistently negative antiphospholipid antibody (aPL) titers, a condition termed seronegative APS (SN-APS). This diagnosis, often one of exclusion, is considered only after ruling out other inherited and acquired thrombophilic conditions.
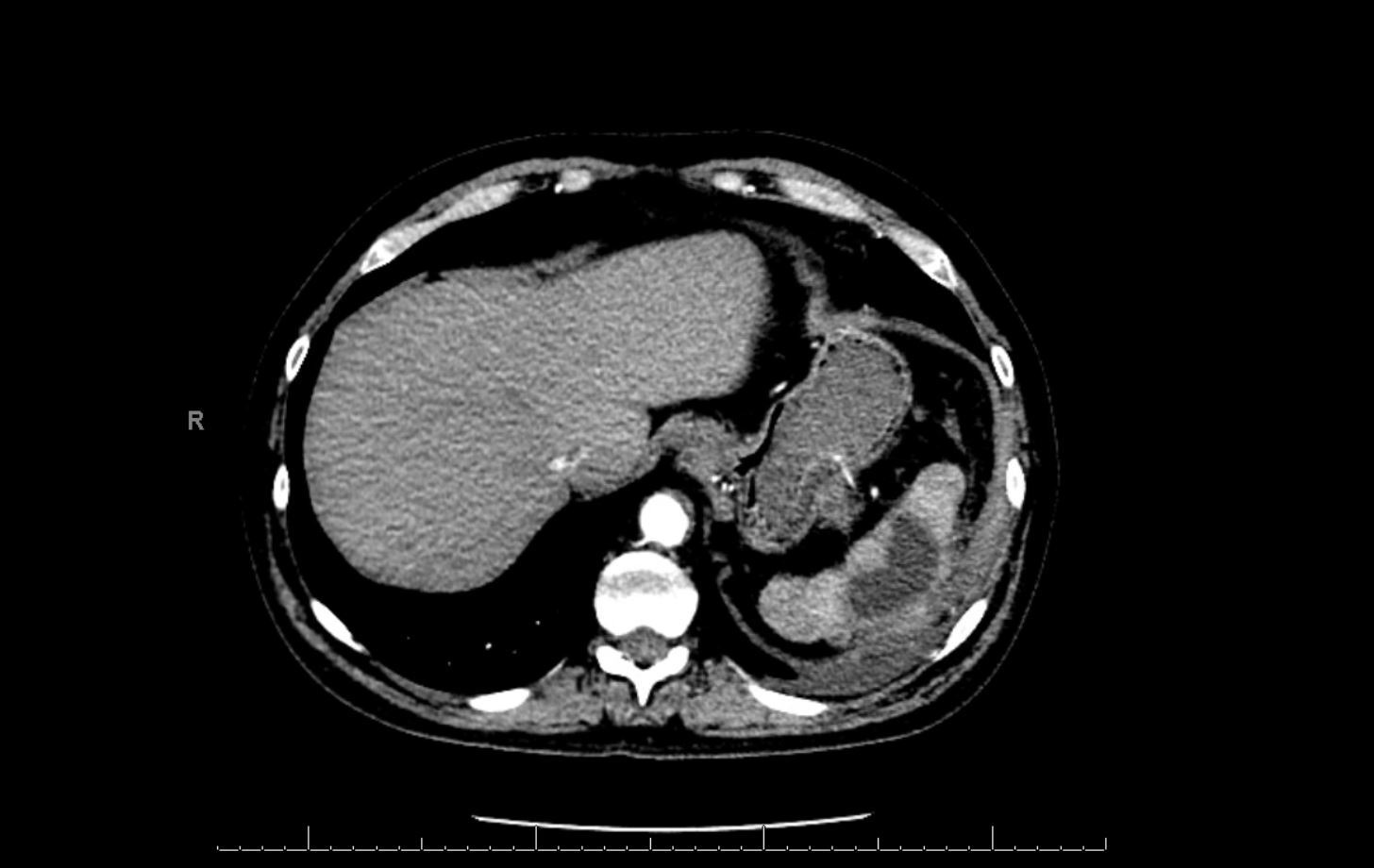
Case Description/Methods: A 45-year-old male with a history of recurrent pulmonary emboli, pancreatitis with pseudocyst, and retinal artery occlusion presented with generalized abdominal pain. Laboratory findings revealed elevated WBC 25k and lipase 60, with other parameters within normal limits. CT abdomen showed a splenic abscess, and CTA identified thrombosis in the splenic artery and superior mesenteric artery (SMA). Seronegative anti-phospholipid syndrome (SN-APS) was suspected due to recurrent thrombotic events despite initial negative aPL tests. He underwent abscess drainage and received empirical treatment with Ceftriaxone and Metronidazole. Management involved transitioning from direct oral anticoagulants to Vitamin K Antagonists for SN-APS, highlighting the importance of personalized therapy and ongoing research for optimal patient care.
Discussion: The initial clinical diagnosis in this patient was based on a history of multiple thrombotic events, starting with pulmonary emboli, followed by ophthalmological complications, and subsequently a splenic abscess and infarct. Differential diagnoses included thrombophilia, malignancy, and disseminated intravascular coagulation (DIC). During hospitalization, aPL testing was initially negative, possibly due to consumption. Over a six-month follow-up post-discharge, laboratory results remained negative for autoimmune diseases, thrombophilia, and infectious diseases. This case highlights the complexity of diagnosing SN-APS, characterized by recurrent thrombosis including involvement of the splenic and superior mesenteric arteries, and challenges in treatment with direct oral anticoagulants (DOACs), emphasizing the importance of personalized therapeutic strategies and ongoing clinical monitoring.
Disclosures:
Sakshi Bai, MD,, Bipneet Singh, MD, Abraham Kisule, MD, Niroshan Ranjan, MD. P1572 - Splenic infarct and SMA thrombosis as a manifestation of Seronegative Antiphospholipid Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Henry Ford Jackson Hospital, Jackson, MI
Introduction: Antiphospholipid Syndrome (APS) presents with a wide spectrum of clinical manifestations, ranging from asymptomatic cases to life-threatening catastrophic APS. Thrombosis in large or micro-vessels can affect virtually any organ system. Diagnostic criteria for APS have evolved, typically requiring the presence of one clinical criterion and one laboratory criterion. However, emerging research highlights cases where patients exhibit clinical features of APS despite transiently positive or persistently negative antiphospholipid antibody (aPL) titers, a condition termed seronegative APS (SN-APS). This diagnosis, often one of exclusion, is considered only after ruling out other inherited and acquired thrombophilic conditions.
Case Description/Methods: A 45-year-old male with a history of recurrent pulmonary emboli, pancreatitis with pseudocyst, and retinal artery occlusion presented with generalized abdominal pain. Laboratory findings revealed elevated WBC 25k and lipase 60, with other parameters within normal limits. CT abdomen showed a splenic abscess, and CTA identified thrombosis in the splenic artery and superior mesenteric artery (SMA). Seronegative anti-phospholipid syndrome (SN-APS) was suspected due to recurrent thrombotic events despite initial negative aPL tests. He underwent abscess drainage and received empirical treatment with Ceftriaxone and Metronidazole. Management involved transitioning from direct oral anticoagulants to Vitamin K Antagonists for SN-APS, highlighting the importance of personalized therapy and ongoing research for optimal patient care.
Discussion: The initial clinical diagnosis in this patient was based on a history of multiple thrombotic events, starting with pulmonary emboli, followed by ophthalmological complications, and subsequently a splenic abscess and infarct. Differential diagnoses included thrombophilia, malignancy, and disseminated intravascular coagulation (DIC). During hospitalization, aPL testing was initially negative, possibly due to consumption. Over a six-month follow-up post-discharge, laboratory results remained negative for autoimmune diseases, thrombophilia, and infectious diseases. This case highlights the complexity of diagnosing SN-APS, characterized by recurrent thrombosis including involvement of the splenic and superior mesenteric arteries, and challenges in treatment with direct oral anticoagulants (DOACs), emphasizing the importance of personalized therapeutic strategies and ongoing clinical monitoring.
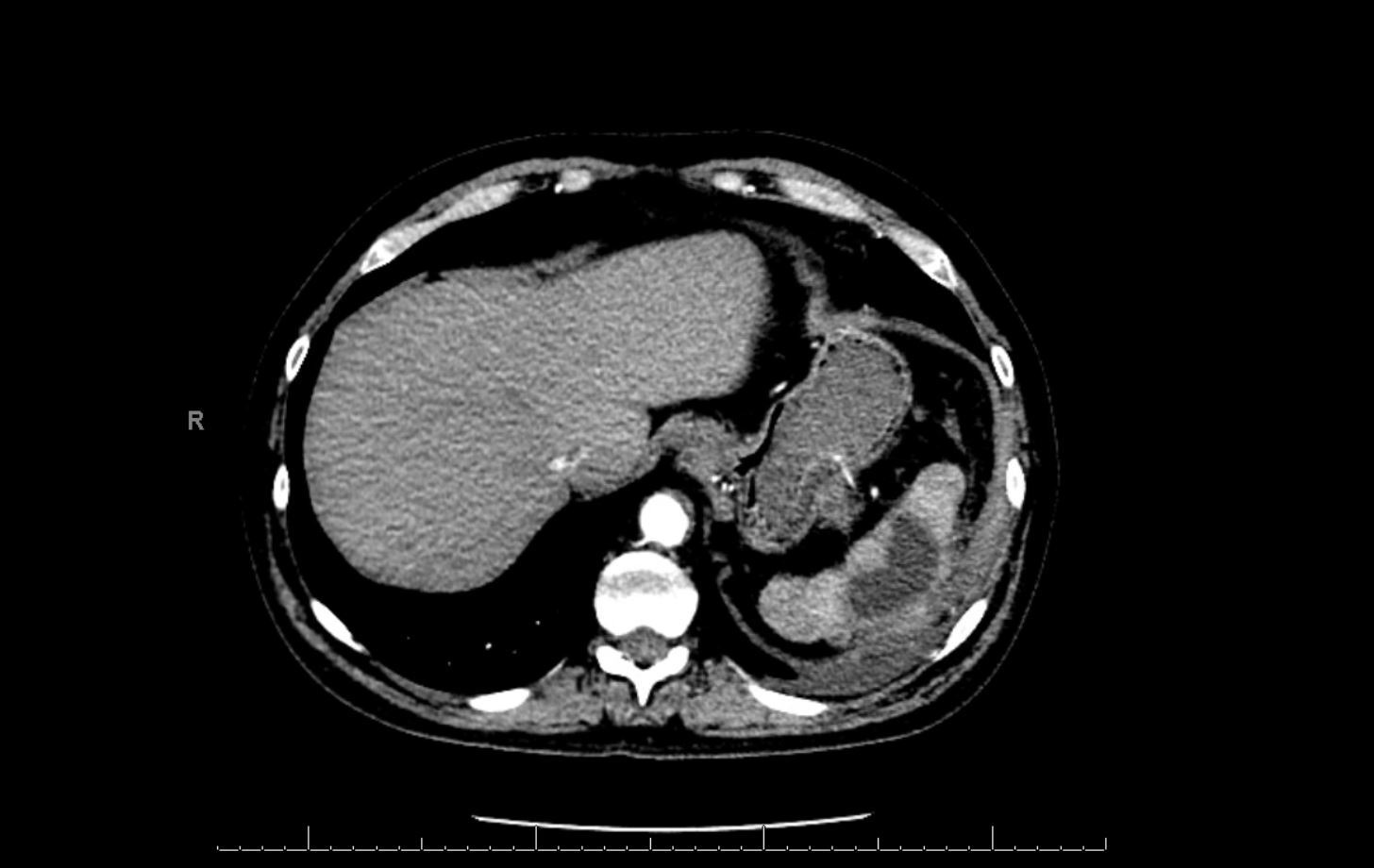
Figure: Splenic abscess
Disclosures:
Sakshi Bai indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Abraham Kisule indicated no relevant financial relationships.
Niroshan Ranjan indicated no relevant financial relationships.
Sakshi Bai, MD,, Bipneet Singh, MD, Abraham Kisule, MD, Niroshan Ranjan, MD. P1572 - Splenic infarct and SMA thrombosis as a manifestation of Seronegative Antiphospholipid Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
