Sunday Poster Session
Category: Small Intestine
P1582 - Gastric Outlet Obstruction Caused by Histoplasmosis in a Non-Endemic Region
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KS
Katherine Shepherd, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Katherine Shepherd, MD1, George Obeng, MD1, Justin T.. Kupec, MD1, William Hsueh, MD2
1West Virginia University, Morgantown, WV; 2Adventist Health Physician Network, Visalia, CA
Introduction: Histoplasmosis capsulatum is a dimorphic fungus present in the soil of the Midwest and commonly considered endemic near the Mississippi and Ohio River regions. However, studies of soil environments suggest there may be a wider geographical area across the United States suitable for growth. Symptoms of histoplasmosis can be mild in immunocompetent patients and can present with disseminated infections affecting multiple organ systems in immunocompromised patients.
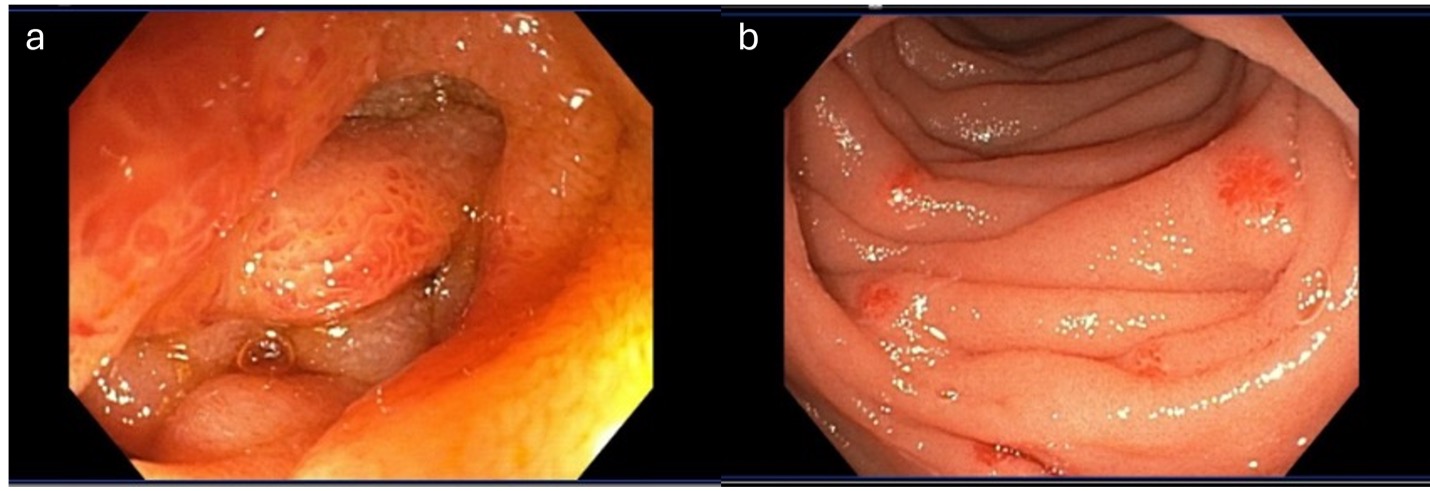
Case Description/Methods: A 29-year-old male with no significant past medical history or recent travel presented to a hospital in San Joaquin Valley, California with refractory nausea and vomiting, chronic diarrhea, and weight loss. He was hypotensive, tachycardic, and had a protuberant abdomen without rigidity or rebound tenderness on exam. Initial workup revealed mild microcytic anemia, normal white blood cell count, positive human immunodeficiency virus (HIV) screen with a viral load of 700,000/mL, and a CD4 count of 1 cells/mm3. Imaging was significant for gastric and duodenal distention with concerns of duodenal stenosis in addition to prominent central mesenteric and retroperitoneal lymphadenopathy. An upper endoscopy was performed which found an 8 mm polypoid lesion located at the gastro-esophageal junction (GEJ) and significant edematous duodenitis as well as scattered erythematous lesions in the duodenum. Biopsies taken of the GEJ lesion and site of duodenal stenosis revealed innumerable small, round yeast cells consistent with H. capsulatum. The patient was started on amphotericin B as well as highly active antiretroviral therapy.
Discussion: Gastrointestinal (GI) involvement is common in patients with disseminated disease, but symptoms are rare. GI involvement with histoplasmosis most commonly occurs in the colon and terminal ileum. The duodenum is seldomly described in the literature as a location of histoplasmosis. Only one other case of histoplasmosis causing gastric outlet obstruction to our knowledge has been reported, and the mechanism is through a pancreatic cyst. This case contributes to the existing literature by describing a clinically symptomatic case with the affected duodenum being the driver of gastric outlet syndrome. We propose histoplasmosis should be considered as a potential fungal infection in a wider geographical region than previously thought and that histoplasmosis should remain on the differential when a patient presents with gastric outlet syndrome.
Disclosures:
Katherine Shepherd, MD1, George Obeng, MD1, Justin T.. Kupec, MD1, William Hsueh, MD2. P1582 - Gastric Outlet Obstruction Caused by Histoplasmosis in a Non-Endemic Region, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2Adventist Health Physician Network, Visalia, CA
Introduction: Histoplasmosis capsulatum is a dimorphic fungus present in the soil of the Midwest and commonly considered endemic near the Mississippi and Ohio River regions. However, studies of soil environments suggest there may be a wider geographical area across the United States suitable for growth. Symptoms of histoplasmosis can be mild in immunocompetent patients and can present with disseminated infections affecting multiple organ systems in immunocompromised patients.
Case Description/Methods: A 29-year-old male with no significant past medical history or recent travel presented to a hospital in San Joaquin Valley, California with refractory nausea and vomiting, chronic diarrhea, and weight loss. He was hypotensive, tachycardic, and had a protuberant abdomen without rigidity or rebound tenderness on exam. Initial workup revealed mild microcytic anemia, normal white blood cell count, positive human immunodeficiency virus (HIV) screen with a viral load of 700,000/mL, and a CD4 count of 1 cells/mm3. Imaging was significant for gastric and duodenal distention with concerns of duodenal stenosis in addition to prominent central mesenteric and retroperitoneal lymphadenopathy. An upper endoscopy was performed which found an 8 mm polypoid lesion located at the gastro-esophageal junction (GEJ) and significant edematous duodenitis as well as scattered erythematous lesions in the duodenum. Biopsies taken of the GEJ lesion and site of duodenal stenosis revealed innumerable small, round yeast cells consistent with H. capsulatum. The patient was started on amphotericin B as well as highly active antiretroviral therapy.
Discussion: Gastrointestinal (GI) involvement is common in patients with disseminated disease, but symptoms are rare. GI involvement with histoplasmosis most commonly occurs in the colon and terminal ileum. The duodenum is seldomly described in the literature as a location of histoplasmosis. Only one other case of histoplasmosis causing gastric outlet obstruction to our knowledge has been reported, and the mechanism is through a pancreatic cyst. This case contributes to the existing literature by describing a clinically symptomatic case with the affected duodenum being the driver of gastric outlet syndrome. We propose histoplasmosis should be considered as a potential fungal infection in a wider geographical region than previously thought and that histoplasmosis should remain on the differential when a patient presents with gastric outlet syndrome.
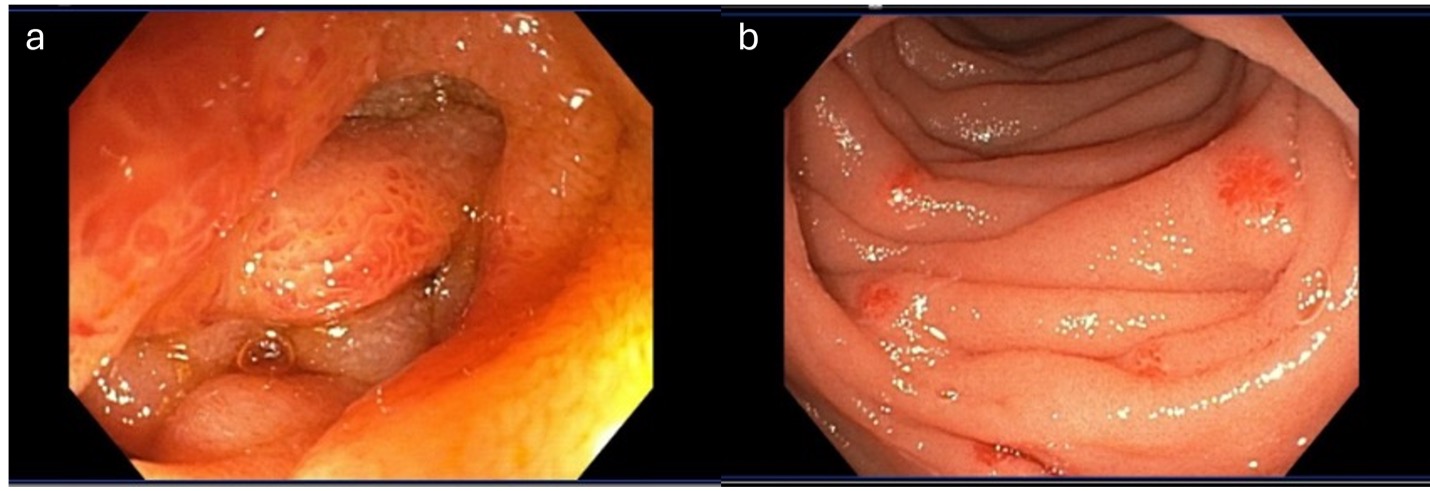
Figure: Figure 1: Endoscopic image showing edematous duodenitis with stenosis (a) and multiple, round erythematous lesions in the duodenum (b).
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
George Obeng indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
William Hsueh indicated no relevant financial relationships.
Katherine Shepherd, MD1, George Obeng, MD1, Justin T.. Kupec, MD1, William Hsueh, MD2. P1582 - Gastric Outlet Obstruction Caused by Histoplasmosis in a Non-Endemic Region, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
