Sunday Poster Session
Category: Stomach
P1637 - A Rare Case of Gastric Necrosis Post-Cardiac Arrest
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Porsha Okiye, MD, MS, MD
Augusta University Medical Center
Augusta, GA
Presenting Author(s)
Porsha Okiye, MD, MS, MD1, Amit Hudgi, MD2, Amol Sharma, MS, MD, FACG3, Anam Herekar, MD2
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Gastrointestinal bleeding due to ischemia following cardiopulmonary resuscitation is rare, but associated with high mortality. The stomach has a rich collateral blood supply and therefore, gastric necrosis is rare. We report the first case of gastric necrosis after cardiac arrest with successful resuscitation.
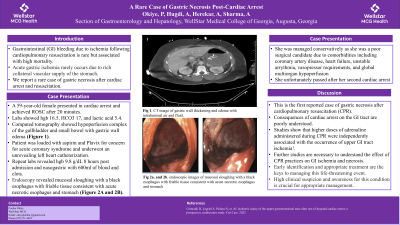
Case Description/Methods: A 59-year-old female with a past medical history of coronary artery disease and congestive heart failure presented in cardiac arrest enroute to the emergency department. ACLS was initiated and a return of spontaneous circulation was obtained after 20 minutes of resuscitation measures. Initial labs were significant for WBC 7.4, Hgb 16.1, HCO3 17, glucose 503, Lactic acid 5.4. CT abdomen and pelvis was suggestive of a hypoperfusion complex of the gallbladder, adrenal glands, left kidney, and small bowel seen in Figure 1.
The patient was given aspirin and Plavix for acute coronary syndrome and subsequently underwent an unrevealing left heart catheterization without any obstructive lesions.
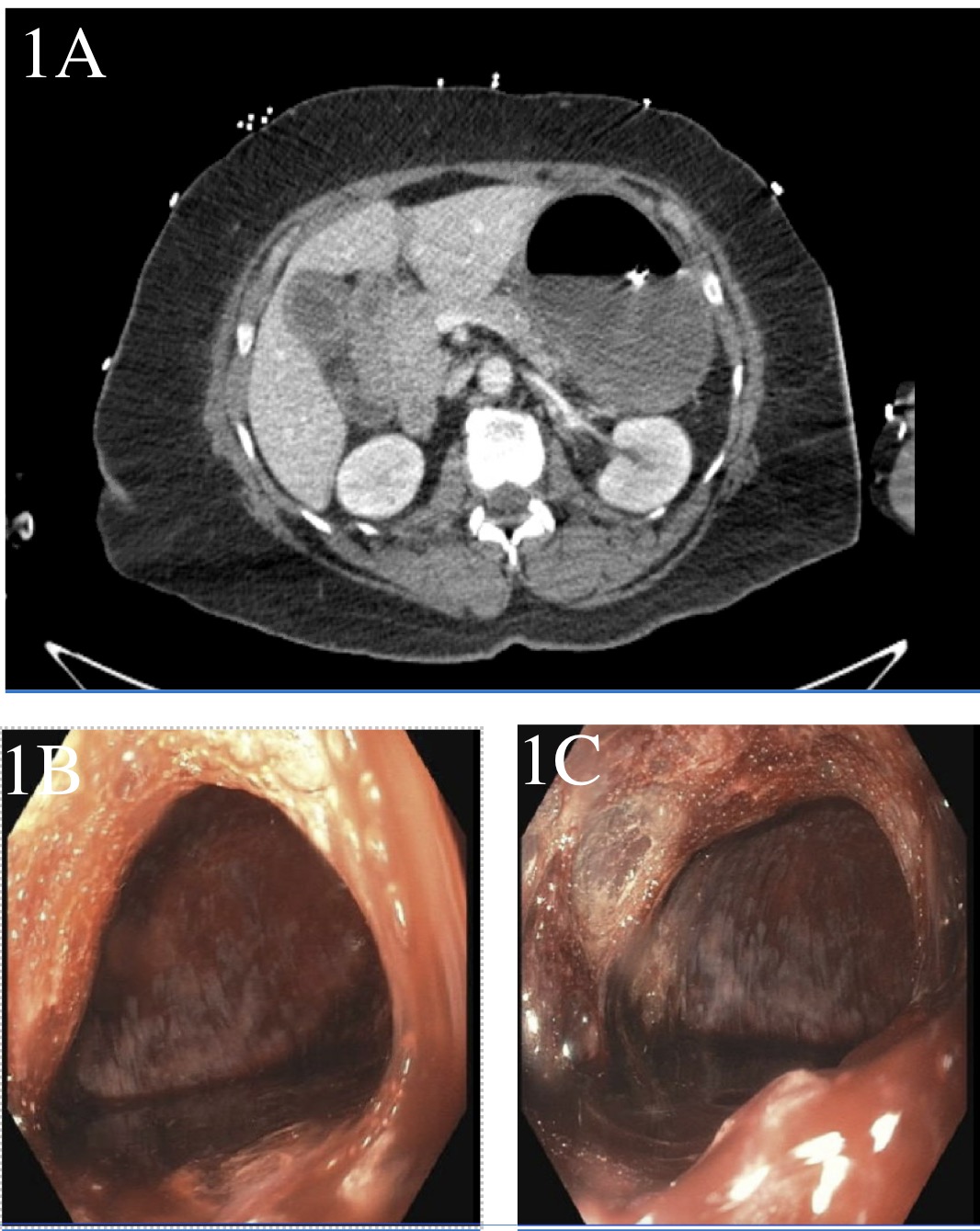
Repeat labs showed a decrease in hemoglobin from 16.5 g/dL on admission to 9.8 g/dL within 8 hours after admission and her nasogastric tube had 600ml of bloody output with clots. She was started on intravenous pantoprazole. An urgent EGD revealed severe mucosal sloughing with a black esophagus with exposed underlying friable tissue consistent with acute necrotic esophagus and necrotic stomach with mucosal sloughing with exposed underlying friable tissue shown in Figure 2.
The patient was not a candidate for surgical intervention and was managed conservatively with supportive care. Despite aggressive resuscitation, her clinical status worsened, and she unfortunately succumbed to a subsequent cardiac arrest during her hospitalization.
Discussion: This is the first reported case of gastric necrosis after cardiopulmonary resuscitation. The consequences of cardiac arrest on the GI tract are poorly understood. A prospective study demonstrated that higher doses of adrenaline administered during CPR were independently associated with the occurrence of upper GI tract ischemia.1 This case highlights the need for further studies to better understand the effect of CPR practices on GI ischemia and necrosis.
Disclosures:
Porsha Okiye, MD, MS, MD1, Amit Hudgi, MD2, Amol Sharma, MS, MD, FACG3, Anam Herekar, MD2. P1637 - A Rare Case of Gastric Necrosis Post-Cardiac Arrest, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Gastrointestinal bleeding due to ischemia following cardiopulmonary resuscitation is rare, but associated with high mortality. The stomach has a rich collateral blood supply and therefore, gastric necrosis is rare. We report the first case of gastric necrosis after cardiac arrest with successful resuscitation.
Case Description/Methods: A 59-year-old female with a past medical history of coronary artery disease and congestive heart failure presented in cardiac arrest enroute to the emergency department. ACLS was initiated and a return of spontaneous circulation was obtained after 20 minutes of resuscitation measures. Initial labs were significant for WBC 7.4, Hgb 16.1, HCO3 17, glucose 503, Lactic acid 5.4. CT abdomen and pelvis was suggestive of a hypoperfusion complex of the gallbladder, adrenal glands, left kidney, and small bowel seen in Figure 1.
The patient was given aspirin and Plavix for acute coronary syndrome and subsequently underwent an unrevealing left heart catheterization without any obstructive lesions.
Repeat labs showed a decrease in hemoglobin from 16.5 g/dL on admission to 9.8 g/dL within 8 hours after admission and her nasogastric tube had 600ml of bloody output with clots. She was started on intravenous pantoprazole. An urgent EGD revealed severe mucosal sloughing with a black esophagus with exposed underlying friable tissue consistent with acute necrotic esophagus and necrotic stomach with mucosal sloughing with exposed underlying friable tissue shown in Figure 2.
The patient was not a candidate for surgical intervention and was managed conservatively with supportive care. Despite aggressive resuscitation, her clinical status worsened, and she unfortunately succumbed to a subsequent cardiac arrest during her hospitalization.
Discussion: This is the first reported case of gastric necrosis after cardiopulmonary resuscitation. The consequences of cardiac arrest on the GI tract are poorly understood. A prospective study demonstrated that higher doses of adrenaline administered during CPR were independently associated with the occurrence of upper GI tract ischemia.1 This case highlights the need for further studies to better understand the effect of CPR practices on GI ischemia and necrosis.
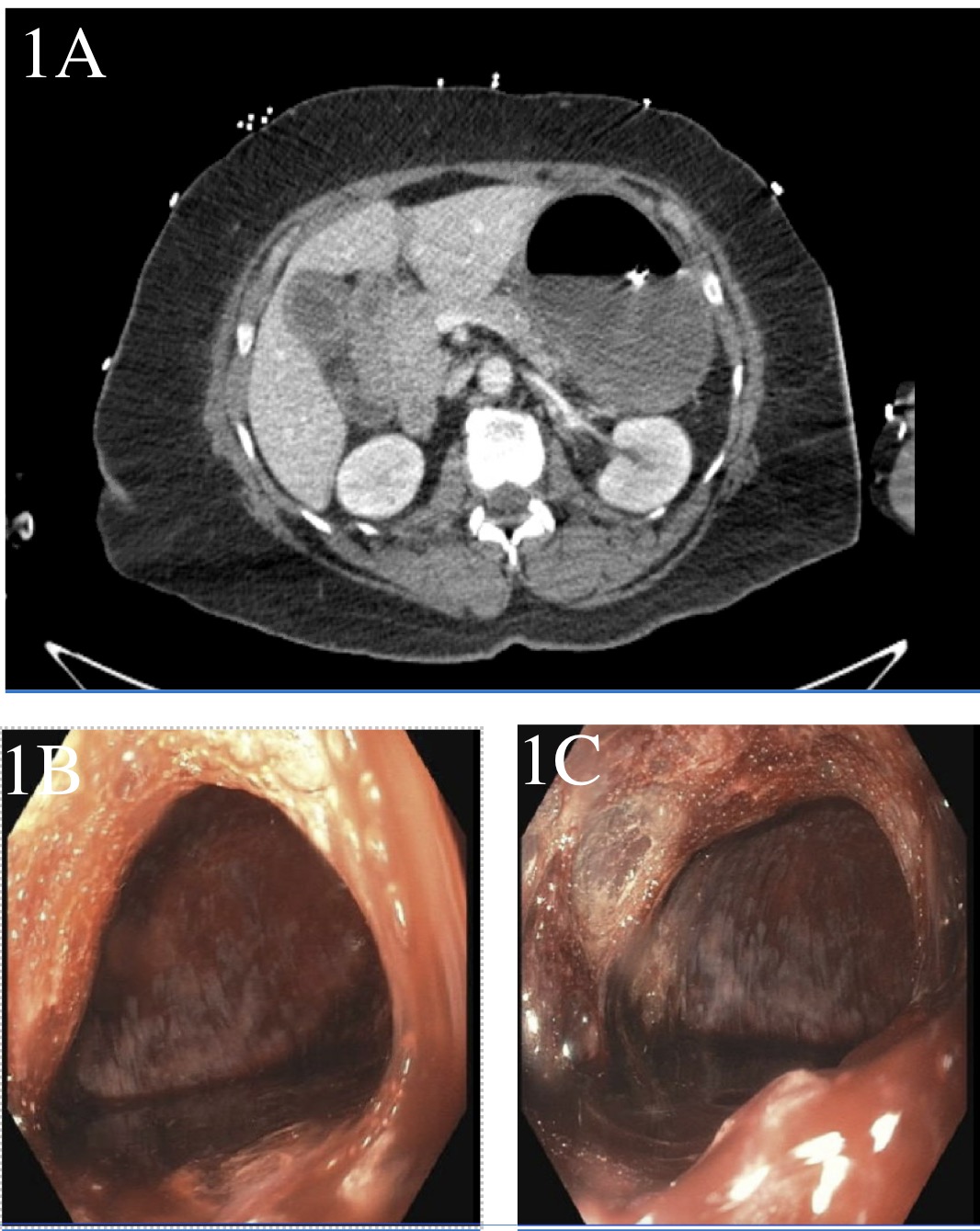
Figure: Figure 1A. Hypoperfusion complex of the gallbladder, adrenal glands, left kidney, and small bowel.
Figure 1B. and 1C. Acute necrotic stomach. Severe gastric inflammation with mucosal sloughing with exposed underlying friable tissue. Blood seen in the stomach likely from oozing of the mucosa
Figure 1B. and 1C. Acute necrotic stomach. Severe gastric inflammation with mucosal sloughing with exposed underlying friable tissue. Blood seen in the stomach likely from oozing of the mucosa
Disclosures:
Porsha Okiye indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Anam Herekar indicated no relevant financial relationships.
Porsha Okiye, MD, MS, MD1, Amit Hudgi, MD2, Amol Sharma, MS, MD, FACG3, Anam Herekar, MD2. P1637 - A Rare Case of Gastric Necrosis Post-Cardiac Arrest, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
