Sunday Poster Session
Category: Stomach
P1645 - Gastroduodenal Intussusception with Gastrointestinal Stromal Tumor (GIST)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Bebawy, DO
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Michael Bebawy, DO1, Mohamed Ismail, DO1, Kranthi Mandava, MD1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Kaveh Hajifathalian, MD1, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, Astoria, NY
Introduction: Gastroduodenal intussusception is a rare condition characterized by the telescoping of a segment of the stomach or duodenum into the adjacent bowel. Upon review of the literature, only 18 cases of intussusception secondary to gastrointestinal stromal tumors (GISTs) were identified.
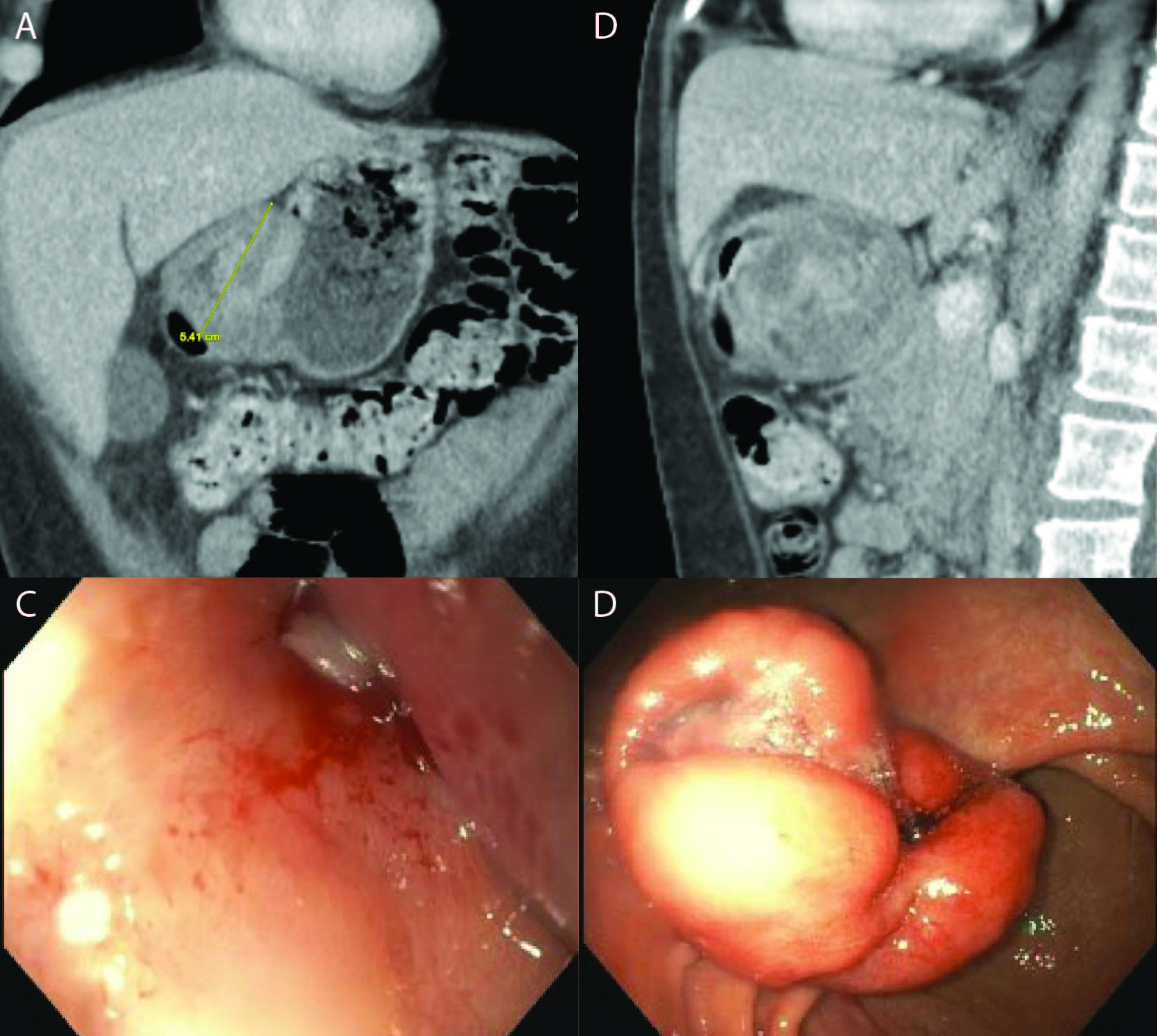
Case Description/Methods: A 53-year-old female with a history of heroin use disorder presented with abdominal pain for two days with associated nausea and vomiting. Initial lab work was remarkable for an elevated lipase. The patient underwent CT abdomen/pelvis which showed gastroduodenal intussusception with a 5 x 4.4 cm lobulated gastric mass serving as a lead point and extending into the proximal duodenum. Additionally, there was concern for secondary obstruction of the pancreatic duct causing acute pancreatitis. Patient underwent EGD, which further demonstrated the gastric mass intussuscepting into the duodenal bulb causing gastric outlet obstruction. The mass was reduced manually with endoscopy and air insufflation. The pathology report showed chronic gastritis; stains for H. Pylori were negative. There was no evidence for malignancy on pathology or immunohistochemical stains. The patient was eventually discharged home with a plan to treat gastritis and repeat endoscopy in 4-6 weeks. A follow-up EGD with endoscopic ultrasound (EUS) was then conducted for deep tissue biopsy due to prior non-diagnostic results. A 33 mm hot snare was used to resect a portion of the mass, which was then submitted for a rush frozen section consistent with a GIST. Immunohistochemical stains were positive for CD117, DOG1, Caldesmon, CD34 and negative for AE1/AE3, desmin, SMA, S100 and SOX10. Subsequently, the patient underwent laparoscopic resection with general surgery.
Discussion: Gastroduodenal intussusception is a unique presentation of a GIST in adults, with few cases having been reported in the literature. This case highlights the diagnostic challenge of identifying gastroduodenal intussusception secondary to gastrointestinal stromal tumors in adults. Immunohistochemical staining played a crucial role in confirming the diagnosis. This allowed for tailored management, including laparoscopic resection without indication for targeted monoclonal antibody therapy. Further research is warranted to better understand the epidemiology, diagnostic approach, and optimal management strategies for gastroduodenal intussusception secondary to GIST in adult populations.
Disclosures:
Michael Bebawy, DO1, Mohamed Ismail, DO1, Kranthi Mandava, MD1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Kaveh Hajifathalian, MD1, Ahmed Al-Khazraji, MD1. P1645 - Gastroduodenal Intussusception with Gastrointestinal Stromal Tumor (GIST), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, Astoria, NY
Introduction: Gastroduodenal intussusception is a rare condition characterized by the telescoping of a segment of the stomach or duodenum into the adjacent bowel. Upon review of the literature, only 18 cases of intussusception secondary to gastrointestinal stromal tumors (GISTs) were identified.
Case Description/Methods: A 53-year-old female with a history of heroin use disorder presented with abdominal pain for two days with associated nausea and vomiting. Initial lab work was remarkable for an elevated lipase. The patient underwent CT abdomen/pelvis which showed gastroduodenal intussusception with a 5 x 4.4 cm lobulated gastric mass serving as a lead point and extending into the proximal duodenum. Additionally, there was concern for secondary obstruction of the pancreatic duct causing acute pancreatitis. Patient underwent EGD, which further demonstrated the gastric mass intussuscepting into the duodenal bulb causing gastric outlet obstruction. The mass was reduced manually with endoscopy and air insufflation. The pathology report showed chronic gastritis; stains for H. Pylori were negative. There was no evidence for malignancy on pathology or immunohistochemical stains. The patient was eventually discharged home with a plan to treat gastritis and repeat endoscopy in 4-6 weeks. A follow-up EGD with endoscopic ultrasound (EUS) was then conducted for deep tissue biopsy due to prior non-diagnostic results. A 33 mm hot snare was used to resect a portion of the mass, which was then submitted for a rush frozen section consistent with a GIST. Immunohistochemical stains were positive for CD117, DOG1, Caldesmon, CD34 and negative for AE1/AE3, desmin, SMA, S100 and SOX10. Subsequently, the patient underwent laparoscopic resection with general surgery.
Discussion: Gastroduodenal intussusception is a unique presentation of a GIST in adults, with few cases having been reported in the literature. This case highlights the diagnostic challenge of identifying gastroduodenal intussusception secondary to gastrointestinal stromal tumors in adults. Immunohistochemical staining played a crucial role in confirming the diagnosis. This allowed for tailored management, including laparoscopic resection without indication for targeted monoclonal antibody therapy. Further research is warranted to better understand the epidemiology, diagnostic approach, and optimal management strategies for gastroduodenal intussusception secondary to GIST in adult populations.
Figure: Figure A – CT abdomen/pelvis coronal view
Figure B – CT abdomen/pelvis sagittal view
CT scan findings demonstrate a 5 cm lobulated gastric mass serving as a lead point and extending into the proximal duodenum.
Figure C – Duodenal bulb
Figure D – Incisura of the Stomach
EGD findings demonstrate a large, ulcerated, non-circumferential mass with no bleeding found at the incisura. The gastric mass was discovered intussuscepting into the duodenal bulb causing a gastric outlet obstruction. The mass was reduced back into the stomach manually with endoscopy and air insufflation.
Figure B – CT abdomen/pelvis sagittal view
CT scan findings demonstrate a 5 cm lobulated gastric mass serving as a lead point and extending into the proximal duodenum.
Figure C – Duodenal bulb
Figure D – Incisura of the Stomach
EGD findings demonstrate a large, ulcerated, non-circumferential mass with no bleeding found at the incisura. The gastric mass was discovered intussuscepting into the duodenal bulb causing a gastric outlet obstruction. The mass was reduced back into the stomach manually with endoscopy and air insufflation.
Disclosures:
Michael Bebawy indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Shivani Patel indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Michael Bebawy, DO1, Mohamed Ismail, DO1, Kranthi Mandava, MD1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Kaveh Hajifathalian, MD1, Ahmed Al-Khazraji, MD1. P1645 - Gastroduodenal Intussusception with Gastrointestinal Stromal Tumor (GIST), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
