Sunday Poster Session
Category: Stomach
P1646 - A Mass Effect of Gastric Adenocarcinoma Causing Obstructive Jaundice
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Rachel Patel, DO
Lehigh Valley Health Network
Coopersburg, PA
Presenting Author(s)
Rachel Patel, DO1, Yash Rao, DO2, Tyler Wark, DO2, Salman Ahmed, DO2, Dominic Parfianowicz, DO2, Shashin Shah, MD3
1Lehigh Valley Health Network, Coopersburg, PA; 2Lehigh Valley Health Network, Allentown, PA; 3Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Gastric cancer is the 5th most diagnosed and 3rd leading cause of cancer deaths globally. Gastric adenocarcinoma presenting as obstructive jaundice is extremely rare, and usually occurs in the context of metastasis to periportal lymph nodes. Here we present a case of primary gastric adenocarcinoma causing obstructive jaundice due to a direct invasion.
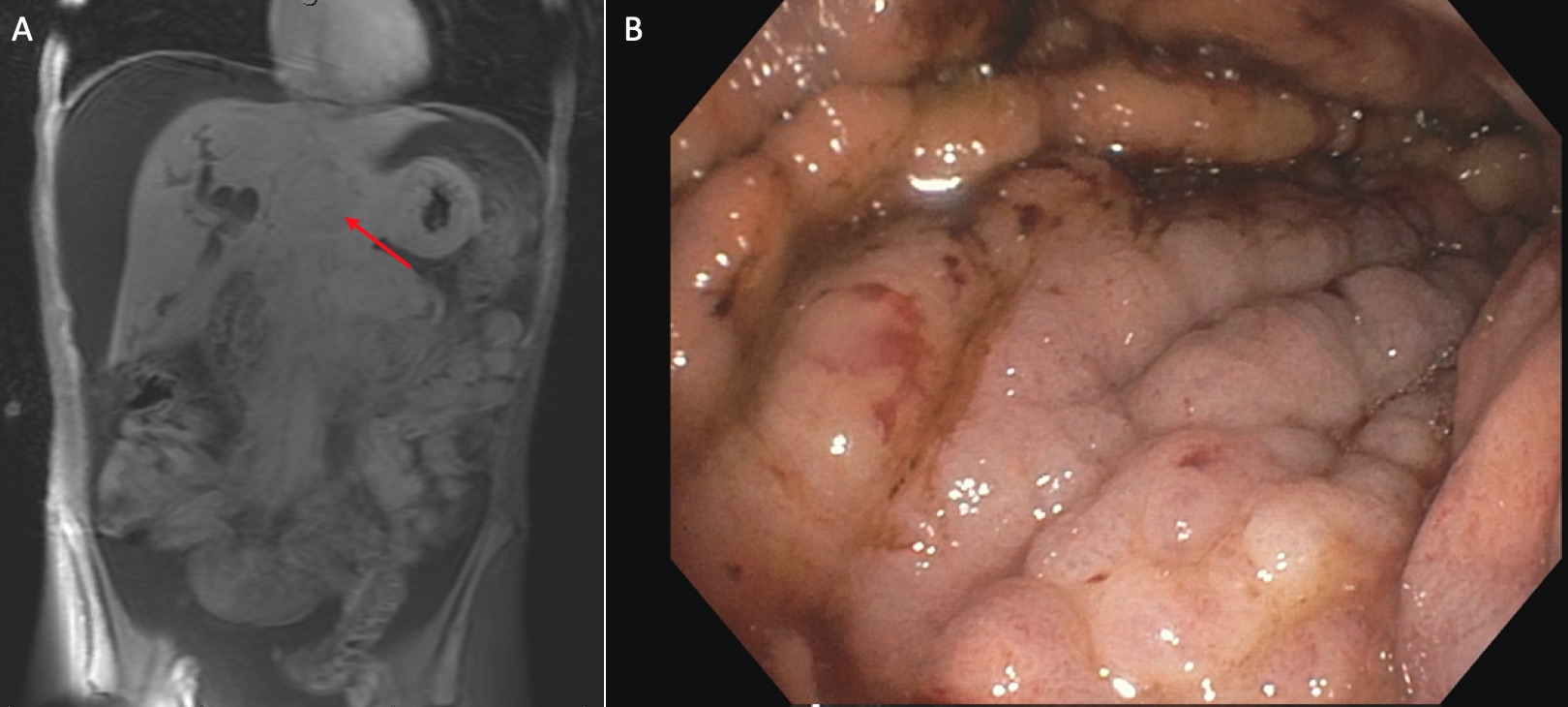
Case Description/Methods: A 40-year-old male with no past medical history presented with jaundice, abdominal pain, and unintentional 20 lb weight loss. Initial labs revealed a total bilirubin of 18.9 mg/dL, direct bilirubin of 9.1 mg/dL, AST 200 U/L, ALT 321 U/L, ALP 1237 U/L, and CA 19-9 1617 U/ml. Abdominal CT showed marked intrahepatic and extrahepatic biliary dilatation with limited evaluation at the confluence of the pancreatic head and CBD that was concerning for biliary or pancreatic malignancy. Evaluation with EGD revealed a firm infiltrating mass 40 cm into the esophagus extending to the GE-junction and encompassing the proximal gastric cardia, fundus, and body. Unfortunately, massive hypertrophy of the gastric body folds prevented insufflation of the stomach, and subsequent ERCP, as the probe could not be passed through the pylorus. EUS showed a dilated biliary tree and 18 mm gastric wall thickening. Biopsies taken from the GE junction and the gastric wall were positive for poorly differentiated adenocarcinoma. He later underwent a MRCP which re-demonstrated an infiltrative mass at the GE junction with mass effect on the porta hepatis causing biliary duct dilatation. Two percutaneous biliary stents were placed for palliative measures. However, due to persistent hyperbilirubinemia, he was deemed not a candidate for chemotherapy and discharged to home hospice.
Discussion: Gastric adenocarcinoma is the most prevalent of gastric cancers, accounting for 6% of total cancer incidence. The presence of obstructive jaundice in a known case of gastric adenocarcinoma should warrant a search for hepatoduodenal lymphadenopathy, bile wall thickening, and liver metastasis. In a study by Lee et. al which reviewed 54 patients, the cause of obstructive jaundice in 50 patients with gastric adenocarcinoma was found to be secondary to metastatic lymphadenopathy to the hepatoduodenal ligament, while the remaining four were found to be from direct invasion of the distal CBD. Mass effect by an aggressive and locally invasive primary gastric adenocarcinoma on the biliary system causing obstructive jaundice as described in our patient above is exceedingly rare.
Disclosures:
Rachel Patel, DO1, Yash Rao, DO2, Tyler Wark, DO2, Salman Ahmed, DO2, Dominic Parfianowicz, DO2, Shashin Shah, MD3. P1646 - A Mass Effect of Gastric Adenocarcinoma Causing Obstructive Jaundice, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lehigh Valley Health Network, Coopersburg, PA; 2Lehigh Valley Health Network, Allentown, PA; 3Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Gastric cancer is the 5th most diagnosed and 3rd leading cause of cancer deaths globally. Gastric adenocarcinoma presenting as obstructive jaundice is extremely rare, and usually occurs in the context of metastasis to periportal lymph nodes. Here we present a case of primary gastric adenocarcinoma causing obstructive jaundice due to a direct invasion.
Case Description/Methods: A 40-year-old male with no past medical history presented with jaundice, abdominal pain, and unintentional 20 lb weight loss. Initial labs revealed a total bilirubin of 18.9 mg/dL, direct bilirubin of 9.1 mg/dL, AST 200 U/L, ALT 321 U/L, ALP 1237 U/L, and CA 19-9 1617 U/ml. Abdominal CT showed marked intrahepatic and extrahepatic biliary dilatation with limited evaluation at the confluence of the pancreatic head and CBD that was concerning for biliary or pancreatic malignancy. Evaluation with EGD revealed a firm infiltrating mass 40 cm into the esophagus extending to the GE-junction and encompassing the proximal gastric cardia, fundus, and body. Unfortunately, massive hypertrophy of the gastric body folds prevented insufflation of the stomach, and subsequent ERCP, as the probe could not be passed through the pylorus. EUS showed a dilated biliary tree and 18 mm gastric wall thickening. Biopsies taken from the GE junction and the gastric wall were positive for poorly differentiated adenocarcinoma. He later underwent a MRCP which re-demonstrated an infiltrative mass at the GE junction with mass effect on the porta hepatis causing biliary duct dilatation. Two percutaneous biliary stents were placed for palliative measures. However, due to persistent hyperbilirubinemia, he was deemed not a candidate for chemotherapy and discharged to home hospice.
Discussion: Gastric adenocarcinoma is the most prevalent of gastric cancers, accounting for 6% of total cancer incidence. The presence of obstructive jaundice in a known case of gastric adenocarcinoma should warrant a search for hepatoduodenal lymphadenopathy, bile wall thickening, and liver metastasis. In a study by Lee et. al which reviewed 54 patients, the cause of obstructive jaundice in 50 patients with gastric adenocarcinoma was found to be secondary to metastatic lymphadenopathy to the hepatoduodenal ligament, while the remaining four were found to be from direct invasion of the distal CBD. Mass effect by an aggressive and locally invasive primary gastric adenocarcinoma on the biliary system causing obstructive jaundice as described in our patient above is exceedingly rare.
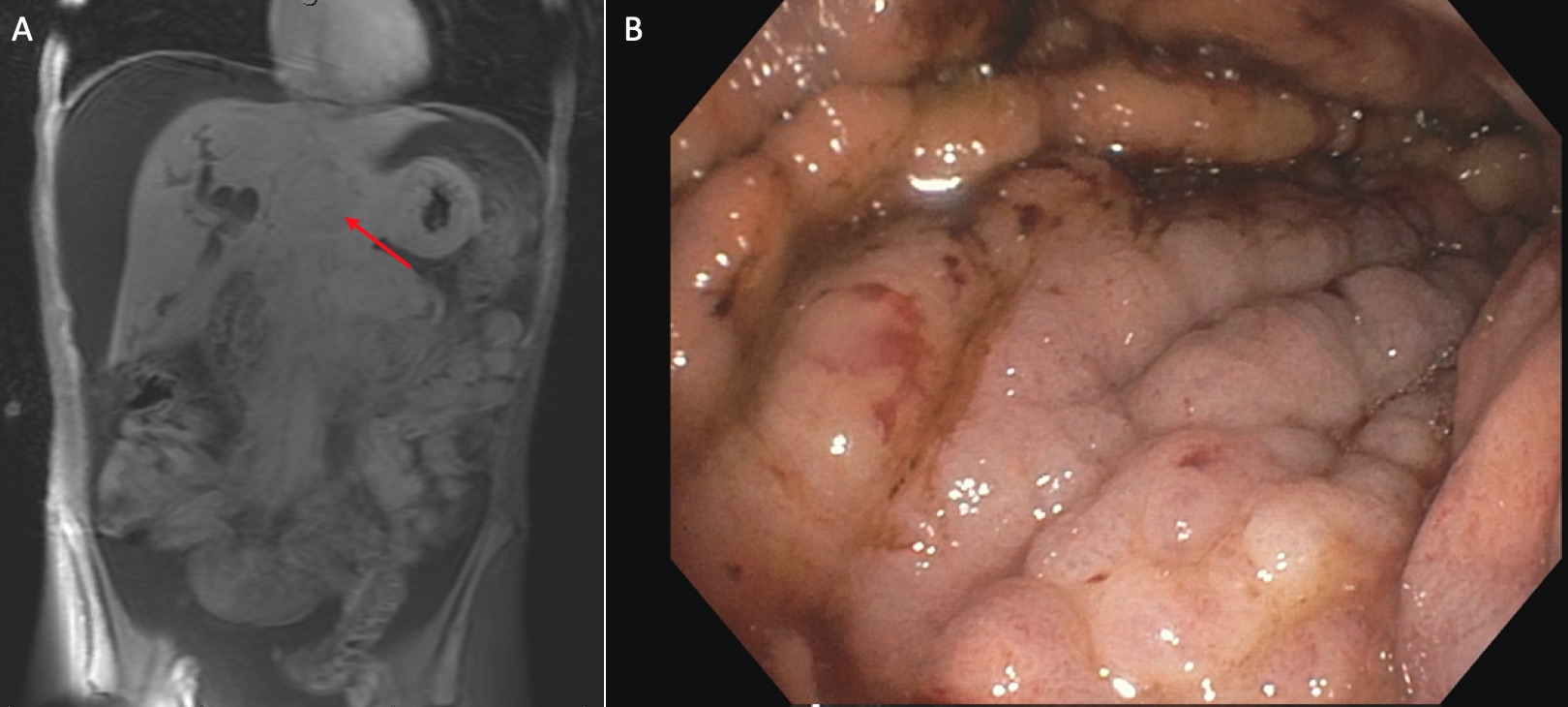
Figure: Image 'A' shows the CT scan of the infiltrating gastric adenocarcinoma causing a mass effect on the biliary system. Image 'B' shows the endoscopy revealing massive hypertrophy of the gastric body folds which restricted the ability of the stomach to insufflate with air.
Disclosures:
Rachel Patel indicated no relevant financial relationships.
Yash Rao indicated no relevant financial relationships.
Tyler Wark indicated no relevant financial relationships.
Salman Ahmed indicated no relevant financial relationships.
Dominic Parfianowicz indicated no relevant financial relationships.
Shashin Shah indicated no relevant financial relationships.
Rachel Patel, DO1, Yash Rao, DO2, Tyler Wark, DO2, Salman Ahmed, DO2, Dominic Parfianowicz, DO2, Shashin Shah, MD3. P1646 - A Mass Effect of Gastric Adenocarcinoma Causing Obstructive Jaundice, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

