Sunday Poster Session
Category: Stomach
P1653 - IR Embolization Wire Causing Trauma and Upper GI Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Malik Mushannen, MD
New York-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Malik Mushannen, MD1, Michelle Lee, MD2, Chimsom Orakwue, MD3, David L. Carr-Locke, MA, MD, FACG4, David Wan, MD3
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 4Weill Cornell Medicine, New York, NY
Introduction: Interventional-radiology guided embolization of GI bleeding can be used to treat large bleeding masses or sources which cannot be managed endoscopically. However, the long-term side effects of coil migration is not well studied. Here we report a case of embolization coils as a cause for upper GI bleeding from a gastric antral tumor.
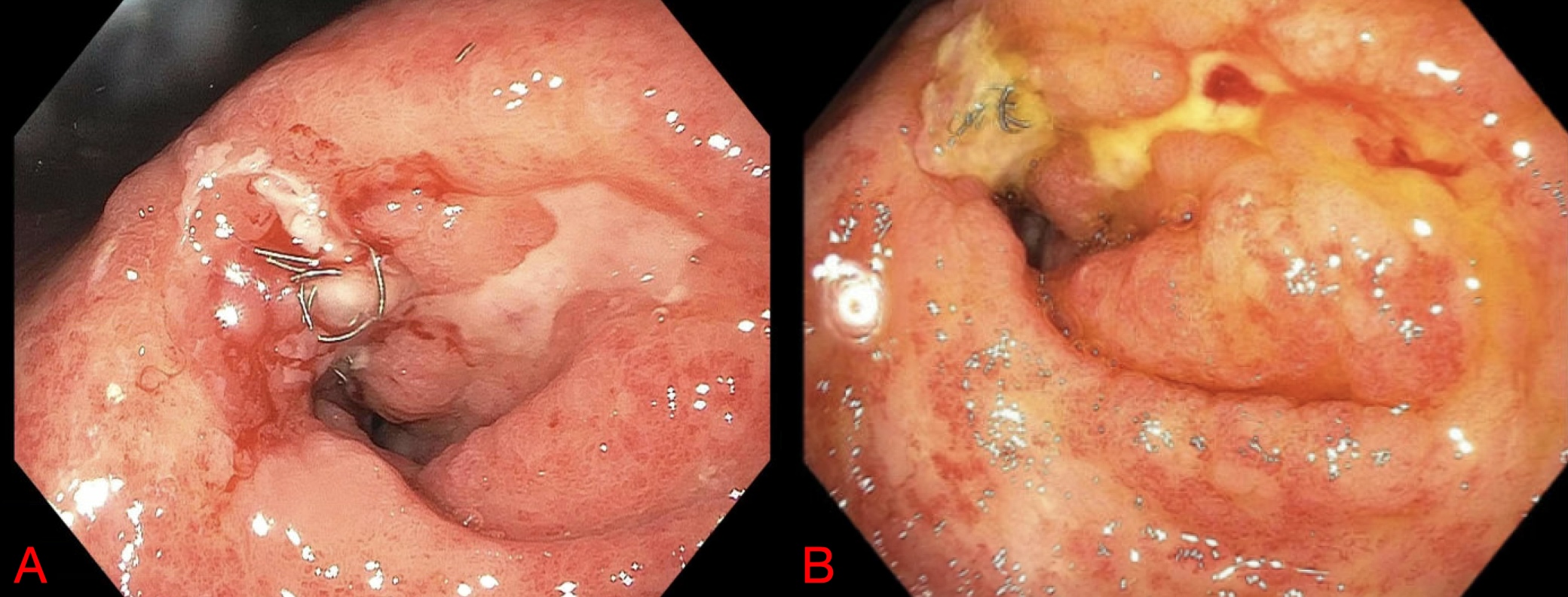
Case Description/Methods: An 84-year-old man with a history of metastatic gastric adenocarcinoma treated with chemotherapy and radiation, complicated by recurrent GI bleeding with subsequent embolization of the superior mesenteric and celiac artery, pulmonary embolism and atrial fibrillation on anticoagulation, presented with generalized fatigue, shortness of breath, and melena for four days. He was found to have worsening anemia, with a hemoglobin 6.2 g/dl from 9.2 g/dl, and underwent upper endoscopy (EGD) which showed an ulcerated circumferential mass with protruding embolization coils that were thought to be causing local irritation of the gastric mass (figure A). The wires were cut with endoscopic scissors and hemostasis was achieved with a surface-acting hemostatic gel.
The patient’s hemoglobin subsequently stabilised and he was discharged, though returned two weeks later again with melena. He underwent repeat endoscopy, showing two red spots of recent bleeding opposite the cut wires, in the gastric mass (figure B). The remaining embolization wire was cut again and electrocautery forceps were used to pull the wire, with subsequent application of surface hemostatic gel.
To avoid recurrent GI bleeding, his anticoagulation was subsequently held and an atrial cage implanted for atrial fibrillation management. Unfortunately, he continued to have episodes of melena with IR guided coils eroding into the mass, and was assessed for a partial gastrectomy. Ultimately, he was considered a poor surgical candidate and is undergoing radiation and immunotherapy with nivolumab.
Discussion: Safety and management of eroding embolization coils when seen during endoscopy and thought to be contributing to GI bleeding is not well defined. We used two different approaches, one with endoscopic scissors and one with electrocautery forceps. However, given the persistent friability of his gastric tumor, the patient continues to have bleeding and erosion from his gastric coils.
Other case reports report the usage of hot biopsy forceps and endoscopic scissors – one involving malignancy. Other case reports have not resulted in persistent subsequent GI bleeding.
Disclosures:
Malik Mushannen, MD1, Michelle Lee, MD2, Chimsom Orakwue, MD3, David L. Carr-Locke, MA, MD, FACG4, David Wan, MD3. P1653 - IR Embolization Wire Causing Trauma and Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 4Weill Cornell Medicine, New York, NY
Introduction: Interventional-radiology guided embolization of GI bleeding can be used to treat large bleeding masses or sources which cannot be managed endoscopically. However, the long-term side effects of coil migration is not well studied. Here we report a case of embolization coils as a cause for upper GI bleeding from a gastric antral tumor.
Case Description/Methods: An 84-year-old man with a history of metastatic gastric adenocarcinoma treated with chemotherapy and radiation, complicated by recurrent GI bleeding with subsequent embolization of the superior mesenteric and celiac artery, pulmonary embolism and atrial fibrillation on anticoagulation, presented with generalized fatigue, shortness of breath, and melena for four days. He was found to have worsening anemia, with a hemoglobin 6.2 g/dl from 9.2 g/dl, and underwent upper endoscopy (EGD) which showed an ulcerated circumferential mass with protruding embolization coils that were thought to be causing local irritation of the gastric mass (figure A). The wires were cut with endoscopic scissors and hemostasis was achieved with a surface-acting hemostatic gel.
The patient’s hemoglobin subsequently stabilised and he was discharged, though returned two weeks later again with melena. He underwent repeat endoscopy, showing two red spots of recent bleeding opposite the cut wires, in the gastric mass (figure B). The remaining embolization wire was cut again and electrocautery forceps were used to pull the wire, with subsequent application of surface hemostatic gel.
To avoid recurrent GI bleeding, his anticoagulation was subsequently held and an atrial cage implanted for atrial fibrillation management. Unfortunately, he continued to have episodes of melena with IR guided coils eroding into the mass, and was assessed for a partial gastrectomy. Ultimately, he was considered a poor surgical candidate and is undergoing radiation and immunotherapy with nivolumab.
Discussion: Safety and management of eroding embolization coils when seen during endoscopy and thought to be contributing to GI bleeding is not well defined. We used two different approaches, one with endoscopic scissors and one with electrocautery forceps. However, given the persistent friability of his gastric tumor, the patient continues to have bleeding and erosion from his gastric coils.
Other case reports report the usage of hot biopsy forceps and endoscopic scissors – one involving malignancy. Other case reports have not resulted in persistent subsequent GI bleeding.
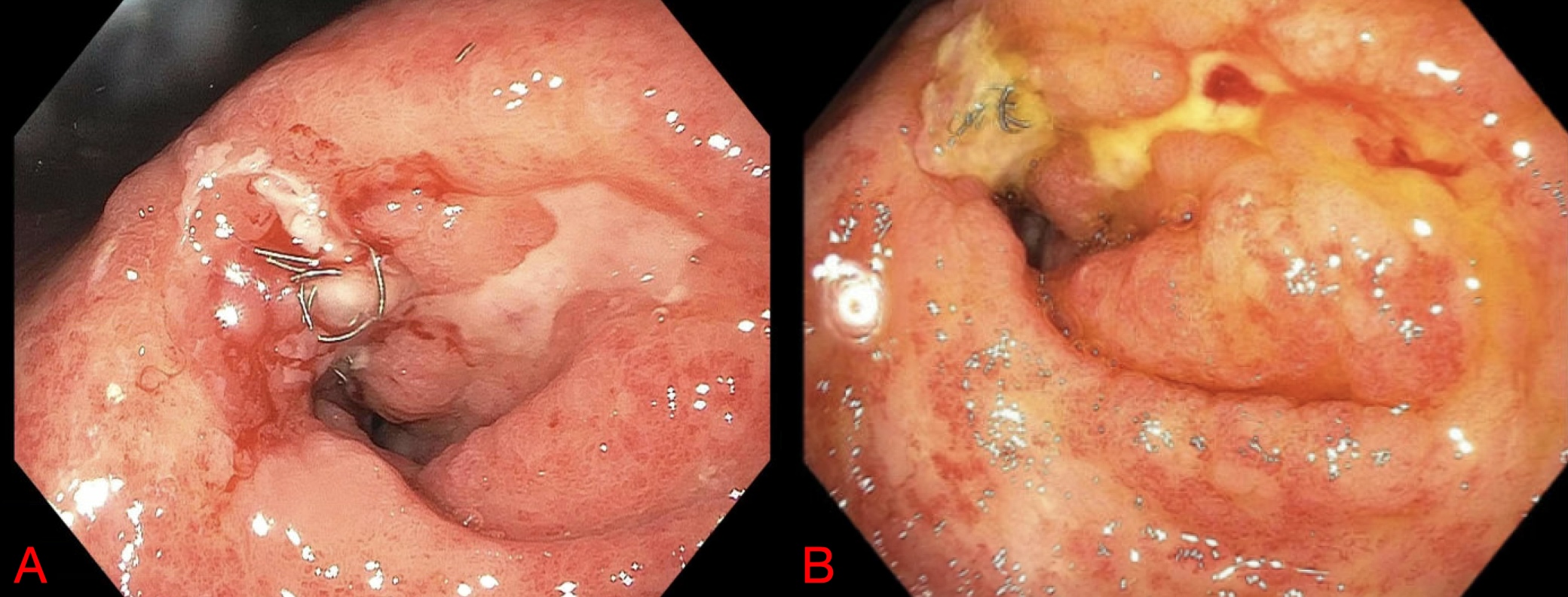
Figure: Figure A: endoscopic finding of coil causing erosion into gastric mass. Performed during first hospital admission
Figure B: repeat endoscopy showing bleeding from gastric mass near coil. Performed during second hospital admission
Figure B: repeat endoscopy showing bleeding from gastric mass near coil. Performed during second hospital admission
Disclosures:
Malik Mushannen indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Chimsom Orakwue indicated no relevant financial relationships.
David Carr-Locke: Steris Corporation – Royalties.
David Wan indicated no relevant financial relationships.
Malik Mushannen, MD1, Michelle Lee, MD2, Chimsom Orakwue, MD3, David L. Carr-Locke, MA, MD, FACG4, David Wan, MD3. P1653 - IR Embolization Wire Causing Trauma and Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

