Sunday Poster Session
Category: Stomach
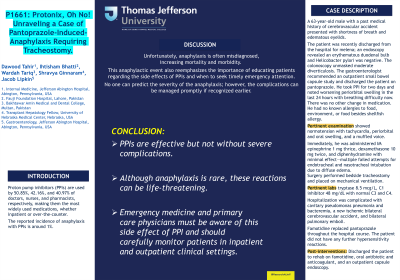
P1661 - Protonix, Oh No! Unraveling a Case of Pantoprazole-Induced-Anaphylaxis Requiring Tracheostomy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Dawood Tahir, MD
Abington Jefferson Hospital
Abington, PA
Presenting Author(s)
Dawood Tahir, MD1, Ihtisham Bhatti, MBBS2, Wardah Tariq, MBBS3, Shravya Ginnaram, MD1, Jacob Lipkin, MD1
1Abington Jefferson Hospital, Abington, PA; 2Fauji Foundation Hospital, Lahore, Punjab, Pakistan; 3Shifa International Hospital, Islamabad, Islamabad, Pakistan
Introduction: Proton pump inhibitors (PPIs) are used by 50.85%, 42.16%, and 40.97% of doctors, nurses, and pharmacists, respectively, making them the most widely used medications, whether inpatient or over-the-counter. The reported incidence of anaphylaxis with PPIs is around 1%.
Case Description/Methods: A 63-year-old male with a past medical history of cerebrovascular accident presented with shortness of breath and edematous eyelids. The patient was recently discharged from the hospital for melena; an endoscopy revealed an erythematous duodenal bulb and Helicobacter pylori was negative. The colonoscopy unmasked moderate diverticulosis. The gastroenterologist recommended an outpatient small bowel capsule study and discharged the patient on pantoprazole. He took PPI for two days and noted worsening periorbital swelling in the last 24 hours with breathing difficulty now. There was no other change in medication. He had no known allergies to food, environment, or food besides shellfish allergy. Pertinent examination showed normotension with tachycardia, periorbital and oral swelling, and a muffled voice. Immediately, he was administered IM epinephrine 1 mg thrice, dexamethasone 10 mg twice, and diphenhydramine with minimal effect—multiple failed attempts for endotracheal and nasotracheal intubation due to diffuse edema. Surgery performed bedside tracheostomy and placed on mechanical ventilation. Pertinent labs tryptase 8.5 mcg/L, C1 inhibitor 48 mg/dL with normal C3 and C4 levels. Hospitalization was complicated with cavitary pseudomonas pneumonia and bacteremia, a new ischemic bilateral cerebrovascular accident, and bilateral pulmonary emboli. Famotidine replaced pantoprazole throughout the hospital course. The patient did not have any further hypersensitivity reactions. Post-interventions, we discharged the patient to rehab on famotidine, oral antibiotic and anticoagulant, and an outpatient capsule endoscopy.
Discussion: PPIs are effective but not without severe complications. Unfortunately, anaphylaxis is misdiagnosed, increasing mortality and morbidity. Although anaphylaxis is rare, prescribers should educate patients about this risk with alarming signs mandating emergent attention.
Disclosures:
Dawood Tahir, MD1, Ihtisham Bhatti, MBBS2, Wardah Tariq, MBBS3, Shravya Ginnaram, MD1, Jacob Lipkin, MD1. P1661 - Protonix, Oh No! Unraveling a Case of Pantoprazole-Induced-Anaphylaxis Requiring Tracheostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Abington Jefferson Hospital, Abington, PA; 2Fauji Foundation Hospital, Lahore, Punjab, Pakistan; 3Shifa International Hospital, Islamabad, Islamabad, Pakistan
Introduction: Proton pump inhibitors (PPIs) are used by 50.85%, 42.16%, and 40.97% of doctors, nurses, and pharmacists, respectively, making them the most widely used medications, whether inpatient or over-the-counter. The reported incidence of anaphylaxis with PPIs is around 1%.
Case Description/Methods: A 63-year-old male with a past medical history of cerebrovascular accident presented with shortness of breath and edematous eyelids. The patient was recently discharged from the hospital for melena; an endoscopy revealed an erythematous duodenal bulb and Helicobacter pylori was negative. The colonoscopy unmasked moderate diverticulosis. The gastroenterologist recommended an outpatient small bowel capsule study and discharged the patient on pantoprazole. He took PPI for two days and noted worsening periorbital swelling in the last 24 hours with breathing difficulty now. There was no other change in medication. He had no known allergies to food, environment, or food besides shellfish allergy. Pertinent examination showed normotension with tachycardia, periorbital and oral swelling, and a muffled voice. Immediately, he was administered IM epinephrine 1 mg thrice, dexamethasone 10 mg twice, and diphenhydramine with minimal effect—multiple failed attempts for endotracheal and nasotracheal intubation due to diffuse edema. Surgery performed bedside tracheostomy and placed on mechanical ventilation. Pertinent labs tryptase 8.5 mcg/L, C1 inhibitor 48 mg/dL with normal C3 and C4 levels. Hospitalization was complicated with cavitary pseudomonas pneumonia and bacteremia, a new ischemic bilateral cerebrovascular accident, and bilateral pulmonary emboli. Famotidine replaced pantoprazole throughout the hospital course. The patient did not have any further hypersensitivity reactions. Post-interventions, we discharged the patient to rehab on famotidine, oral antibiotic and anticoagulant, and an outpatient capsule endoscopy.
Discussion: PPIs are effective but not without severe complications. Unfortunately, anaphylaxis is misdiagnosed, increasing mortality and morbidity. Although anaphylaxis is rare, prescribers should educate patients about this risk with alarming signs mandating emergent attention.
Disclosures:
Dawood Tahir indicated no relevant financial relationships.
Ihtisham Bhatti indicated no relevant financial relationships.
Wardah Tariq indicated no relevant financial relationships.
Shravya Ginnaram indicated no relevant financial relationships.
Jacob Lipkin indicated no relevant financial relationships.
Dawood Tahir, MD1, Ihtisham Bhatti, MBBS2, Wardah Tariq, MBBS3, Shravya Ginnaram, MD1, Jacob Lipkin, MD1. P1661 - Protonix, Oh No! Unraveling a Case of Pantoprazole-Induced-Anaphylaxis Requiring Tracheostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

