Sunday Poster Session
Category: Stomach
P1669 - An Unusual Case of Anorexia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Udit Asija, MD
The Wright Center for Graduate Medical Education
throp, PA
Presenting Author(s)
Udit Asija, MD1, Hanna Blaney, MD, MPH2, Sanya Badar, MD3, Seyma Bayram, MD1, Tejas Nikumbh, MD1, Sun A. Kim, MD, PhD2, David Kleiner, MD, PhD2, Vikas Khurana, MD1, Sheila Kumar, MD, MS2
1The Wright Center for Graduate Medical Education, Scranton, PA; 2National Institutes of Health, Bethesda, MD; 3Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Strongyloidiasis, caused by intestinal nematode Strongyloides stercoralis, is typically asymptomatic but can present with intermittent or persistent gastrointestinal symptoms during the enteric phase of parasitic development and maturation reflecting the parasite's ability to invade mucosa. Untreated infection can lead to systemic symptoms including weight loss and cachexia.
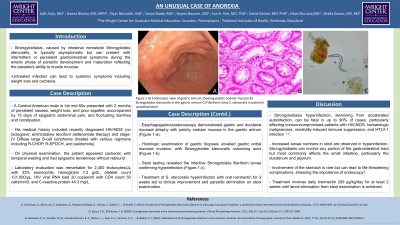
Case Description/Methods: A Central American male in his mid-50s presented with 2 months of persistent nausea, weight loss, and poor appetite, accompanied by 15 days of epigastric abdominal pain, and fluctuating diarrhea and constipation. His medical history included recently diagnosed HIV/AIDS (on bictegravir, emtricitabine tenofovir alafenamide therapy) and stage-IV Diffuse large B-cell lymphoma (treated with various regimens including R-CHOP, R-EPOCH, and palidomide). On physical examination, the patient appeared cachectic with temporal wasting and epigastric tenderness without rebound. Laboratory evaluation was remarkable for 2,400 leukocytes/µL with 33% eosinophils, hemoglobin 7.2 g/dL, platelet count 121,000/µL, HIV viral RNA load 20 copies/ml with CD4 count 50 cells/mm3, and C-reactive protein 44.3 mg/L. Esophagogastroduodenoscopy demonstrated gastric and duodenal mucosal atrophy with patchy nodular mucosa in the gastric antrum (Figure 1-a). Histologic examination of gastric biopsies unveiled gastric antral mucosal invasion, with Strongyloides stercoralis colonizing acini (Figure 1-b). Stool testing revealed the infective Strongyloides filariform larvae confirming hyperinfection (Figure 1-c). Treatment of S. stercoralis hyperinfection with oral ivermectin for 2 weeks led to clinical improvement and parasitic elimination on stool examination.
Discussion: Strongyloidiasis hyperinfection, stemming from accelerated autoinfection, can be fatal in up to 90% of cases, particularly affecting immunocompromised patients with HIV/AIDS, hematologic malignancies, medically-induced immune suppression, and HTLV-1 infection. Increased larvae numbers in stool are observed in hyperinfection. Strongyloidiasis can involve any portion of the gastrointestinal tract but most commonly affects the small intestine, particularly the duodenum and jejunum. Involvement of the stomach is rare but can lead to life-threatening complications, stressing the importance of endoscopy. Treatment involves daily Ivermectin 200 μg/kg/day for at least 2 weeks until larval elimination from stool examination is achieved.

Disclosures:
Udit Asija, MD1, Hanna Blaney, MD, MPH2, Sanya Badar, MD3, Seyma Bayram, MD1, Tejas Nikumbh, MD1, Sun A. Kim, MD, PhD2, David Kleiner, MD, PhD2, Vikas Khurana, MD1, Sheila Kumar, MD, MS2. P1669 - An Unusual Case of Anorexia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Scranton, PA; 2National Institutes of Health, Bethesda, MD; 3Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Strongyloidiasis, caused by intestinal nematode Strongyloides stercoralis, is typically asymptomatic but can present with intermittent or persistent gastrointestinal symptoms during the enteric phase of parasitic development and maturation reflecting the parasite's ability to invade mucosa. Untreated infection can lead to systemic symptoms including weight loss and cachexia.
Case Description/Methods: A Central American male in his mid-50s presented with 2 months of persistent nausea, weight loss, and poor appetite, accompanied by 15 days of epigastric abdominal pain, and fluctuating diarrhea and constipation. His medical history included recently diagnosed HIV/AIDS (on bictegravir, emtricitabine tenofovir alafenamide therapy) and stage-IV Diffuse large B-cell lymphoma (treated with various regimens including R-CHOP, R-EPOCH, and palidomide). On physical examination, the patient appeared cachectic with temporal wasting and epigastric tenderness without rebound. Laboratory evaluation was remarkable for 2,400 leukocytes/µL with 33% eosinophils, hemoglobin 7.2 g/dL, platelet count 121,000/µL, HIV viral RNA load 20 copies/ml with CD4 count 50 cells/mm3, and C-reactive protein 44.3 mg/L. Esophagogastroduodenoscopy demonstrated gastric and duodenal mucosal atrophy with patchy nodular mucosa in the gastric antrum (Figure 1-a). Histologic examination of gastric biopsies unveiled gastric antral mucosal invasion, with Strongyloides stercoralis colonizing acini (Figure 1-b). Stool testing revealed the infective Strongyloides filariform larvae confirming hyperinfection (Figure 1-c). Treatment of S. stercoralis hyperinfection with oral ivermectin for 2 weeks led to clinical improvement and parasitic elimination on stool examination.
Discussion: Strongyloidiasis hyperinfection, stemming from accelerated autoinfection, can be fatal in up to 90% of cases, particularly affecting immunocompromised patients with HIV/AIDS, hematologic malignancies, medically-induced immune suppression, and HTLV-1 infection. Increased larvae numbers in stool are observed in hyperinfection. Strongyloidiasis can involve any portion of the gastrointestinal tract but most commonly affects the small intestine, particularly the duodenum and jejunum. Involvement of the stomach is rare but can lead to life-threatening complications, stressing the importance of endoscopy. Treatment involves daily Ivermectin 200 μg/kg/day for at least 2 weeks until larval elimination from stool examination is achieved.

Figure: Figure 1 A) Endoscopic view of gastric antrum showing patchy nodular mucosa
B) Strongyloides stercoralis in the gastric antrum
C) Filariform larva S. stercoralis in patient’s unstained stool
B) Strongyloides stercoralis in the gastric antrum
C) Filariform larva S. stercoralis in patient’s unstained stool
Disclosures:
Udit Asija indicated no relevant financial relationships.
Hanna Blaney indicated no relevant financial relationships.
Sanya Badar indicated no relevant financial relationships.
Seyma Bayram indicated no relevant financial relationships.
Tejas Nikumbh indicated no relevant financial relationships.
Sun A. Kim indicated no relevant financial relationships.
David Kleiner indicated no relevant financial relationships.
Vikas Khurana indicated no relevant financial relationships.
Sheila Kumar indicated no relevant financial relationships.
Udit Asija, MD1, Hanna Blaney, MD, MPH2, Sanya Badar, MD3, Seyma Bayram, MD1, Tejas Nikumbh, MD1, Sun A. Kim, MD, PhD2, David Kleiner, MD, PhD2, Vikas Khurana, MD1, Sheila Kumar, MD, MS2. P1669 - An Unusual Case of Anorexia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
