Sunday Poster Session
Category: Stomach
P1681 - Genetic Gut Check: Atypical Gastroparesis in an Adult With 10p15.3 Microdeletion Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Jeffrey Li, BA
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Jeffrey Li, BA1, Vismaya S.. Bachu, MD2, Bita Shahrvini, MD1, Mark Baniqued, MD1, Niharika Mallepally, MD, MPH1
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2University of California Los Angeles Medical Center, Los Angeles, CA
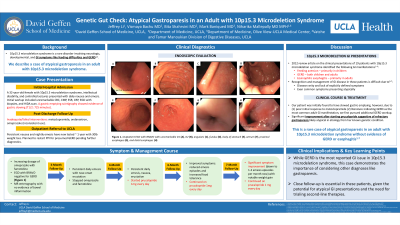
Introduction: 10p15.3 microdeletion syndrome is a rare genetic disorder characterized by neurologic and developmental challenges, along with gastrointestinal (GI) issues like feeding difficulties and gastroesophageal reflux disease (GERD). We describe a case of atypical gastroparesis in an adult patient with 10p15.3 microdeletion syndrome.
Case Description/Methods: A 32-year-old female with 10p15.3 microdeletion syndrome and intellectual disability presented with one year of persistent vomiting and ‘chest pain’ for which a cardiology evaluation was unremarkable. Initial GI workup, including tests for H. pylori, celiac disease, inflammatory bowel disease, a HIDA scan, and EGD with biopsy, were negative. Her symptoms were thought to be from GERD and treated over 4 months with escalating doses of omeprazole, with adjunctive famotidine added later, but without improvement. A subsequent 48-hour intra-esophageal pH study was negative for GERD. By now, the patient had daily emesis and a new 30-lb weight loss. At this point the differential was reconsidered. Gastric emptying scintigraphy revealed delayed emptying. A trial of metoclopramide was unsuccessful. She was then switched to prucalopride which has significantly improved chest pain, emesis, and weight loss.
Discussion: Genetic syndromes – such as 10p15.3 microdeletion syndrome – can affect multiple organ systems and often have GI manifestations. Recognition and management of GI disease in these patients can be difficult due to 1) a lack of explicitly defined symptoms and 2) even common symptoms presenting atypically. In 2012, the first major clinical characterization of 19 patients with 10p15.3 microdeletion syndrome identified 3 pediatric cases with feeding aversion and GERD, attributed to craniofacial dysmorphisms and developmental hypotonia. Our case illustrates an atypical adult presentation of gastroparesis without clear evidence of GERD, expanding the understanding of this condition's GI impact. Another case study described an adult with eosinophilic esophagitis and GERD. Poor feeding is proposed to be from the microdeletion of ZMYND11 and DIP2C genes, potentially impairing enteric nervous system development. Alternatively, some literature blames anatomic abnormalities that mask GI dysmotility. While further research is necessary to better understand 10p15.3 microdeletion syndrome’s pathophysiology, we hope this case raises clinician awareness of atypical GI presentations in such patients and the importance of maintaining a broad differential.
Disclosures:
Jeffrey Li, BA1, Vismaya S.. Bachu, MD2, Bita Shahrvini, MD1, Mark Baniqued, MD1, Niharika Mallepally, MD, MPH1. P1681 - Genetic Gut Check: Atypical Gastroparesis in an Adult With 10p15.3 Microdeletion Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2University of California Los Angeles Medical Center, Los Angeles, CA
Introduction: 10p15.3 microdeletion syndrome is a rare genetic disorder characterized by neurologic and developmental challenges, along with gastrointestinal (GI) issues like feeding difficulties and gastroesophageal reflux disease (GERD). We describe a case of atypical gastroparesis in an adult patient with 10p15.3 microdeletion syndrome.
Case Description/Methods: A 32-year-old female with 10p15.3 microdeletion syndrome and intellectual disability presented with one year of persistent vomiting and ‘chest pain’ for which a cardiology evaluation was unremarkable. Initial GI workup, including tests for H. pylori, celiac disease, inflammatory bowel disease, a HIDA scan, and EGD with biopsy, were negative. Her symptoms were thought to be from GERD and treated over 4 months with escalating doses of omeprazole, with adjunctive famotidine added later, but without improvement. A subsequent 48-hour intra-esophageal pH study was negative for GERD. By now, the patient had daily emesis and a new 30-lb weight loss. At this point the differential was reconsidered. Gastric emptying scintigraphy revealed delayed emptying. A trial of metoclopramide was unsuccessful. She was then switched to prucalopride which has significantly improved chest pain, emesis, and weight loss.
Discussion: Genetic syndromes – such as 10p15.3 microdeletion syndrome – can affect multiple organ systems and often have GI manifestations. Recognition and management of GI disease in these patients can be difficult due to 1) a lack of explicitly defined symptoms and 2) even common symptoms presenting atypically. In 2012, the first major clinical characterization of 19 patients with 10p15.3 microdeletion syndrome identified 3 pediatric cases with feeding aversion and GERD, attributed to craniofacial dysmorphisms and developmental hypotonia. Our case illustrates an atypical adult presentation of gastroparesis without clear evidence of GERD, expanding the understanding of this condition's GI impact. Another case study described an adult with eosinophilic esophagitis and GERD. Poor feeding is proposed to be from the microdeletion of ZMYND11 and DIP2C genes, potentially impairing enteric nervous system development. Alternatively, some literature blames anatomic abnormalities that mask GI dysmotility. While further research is necessary to better understand 10p15.3 microdeletion syndrome’s pathophysiology, we hope this case raises clinician awareness of atypical GI presentations in such patients and the importance of maintaining a broad differential.
Disclosures:
Jeffrey Li indicated no relevant financial relationships.
Vismaya Bachu indicated no relevant financial relationships.
Bita Shahrvini indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Niharika Mallepally indicated no relevant financial relationships.
Jeffrey Li, BA1, Vismaya S.. Bachu, MD2, Bita Shahrvini, MD1, Mark Baniqued, MD1, Niharika Mallepally, MD, MPH1. P1681 - Genetic Gut Check: Atypical Gastroparesis in an Adult With 10p15.3 Microdeletion Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
