Sunday Poster Session
Category: Small Intestine
P1587 - Gastric Intestinal Metaplasia of Duodenum With Subsequent Development of Duodenal Adenoma: An Opportunity for Endoscopic Vigilance
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

- AG
Amlish Gondal, MD
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Amlish Gondal, MD1, Aftab Sharif, MD2, Umer Farooq, MD3, Necat Havlioglu, MD4, Michael Presti, MD5
1Guthrie Robert Packer Hospital, Sayre, PA; 2Saint Mary's Hospital, West Burlington, IA; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4John Cochran VA Medical Center, St. Louis, MO; 5St. Louis Veterans Affairs Medical Center, St. Louis, MO
Introduction: Sporadic non-ampullary duodenal adenomas are detected in patients without familial adenomatous polyposis syndrome with increasing endoscopic visualization. However, progression from duodenal gastric metaplasia remains exceedingly rare with literature
reviews suggesting few case reports.
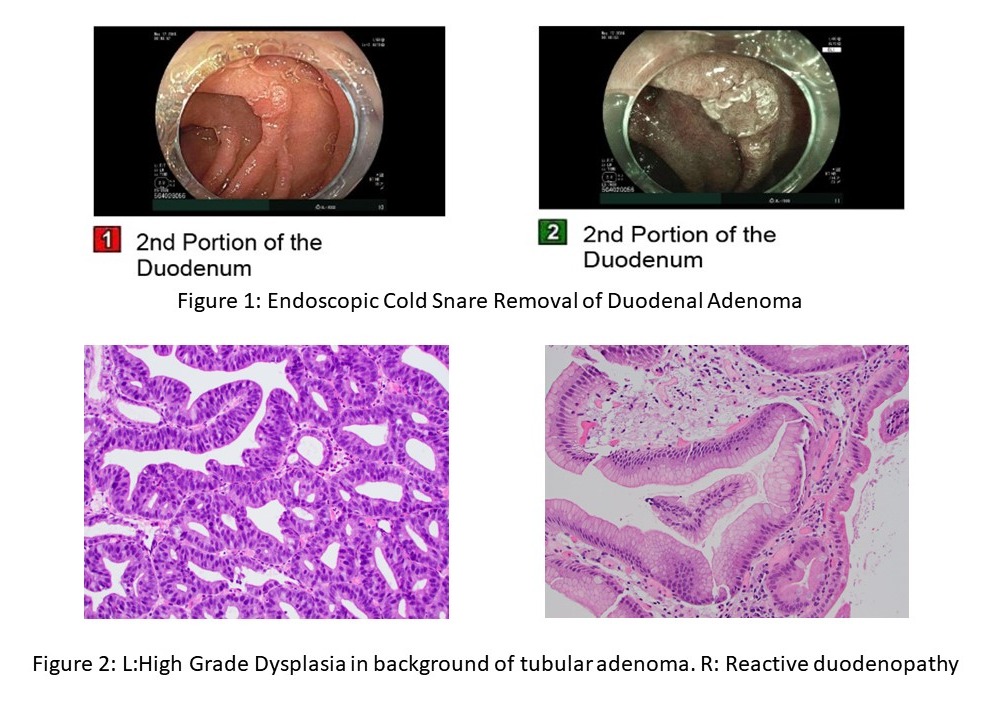
Case Description/Methods: A 49-year-old female presented with epigastric pain with reported improvement after meals. An EGD for duodenal ulcer evaluation was recommended. Patient had a prior history of chronic GERD with short segment Barrett's without dysplasia diagnosed since 2012, IBS-D and chronic anal fissure. A 5 mm non ampullary lesion was seen in the second portion of duodenum- pathology revealed tubular adenoma with focal high-grade dysplasia, random stomach biopsies were negative for H. pylori. She underwent endoscopic cold snare excision of 5 to 6 mm sessile polyp subsequently on a therapeutic EGD with pathology demonstrating high grade dysplasia arising in tubular adenoma (Figure 1, 2). Prior review of endoscopic evaluations revealed that the patient had undergone an EGD about a year before this presentation for workup of diarrhea, celiac disease and IBS-D. Pathology at that time had showed reactive duodenopathy, duodenal mucosa with gastric mucin metaplasia, Brunner's gland hyperplasia and nonspecific chronic inflammation. There was no dysplasia, acute inflammation, granulomas or villous blunting.
Discussion: Gastric metaplasia of duodenum is most often described in context of H. pylori associated gastritis or NSAID use. Progression to duodenal adenoma is rare with most cases of duodenal gastric metaplasia suggesting endoscopic mucosal defects, inflammation, scar. There remains paucity of surveillance and treatment guidelines for this entity in the absence of H. pylori. The present case highlights the necessity of endoscopic vigilance in patients with gastric metaplasia of duodenum. Given established transformation risk to adenocarcinoma and duodenal adenomas, resection with cold snare or EMR, remains recommended for non- ampullary duodenal lesions. However, there are no current guidelines for subsequent endoscopic surveillance gastric metaplasia of duodenum.
Disclosures:
Amlish Gondal, MD1, Aftab Sharif, MD2, Umer Farooq, MD3, Necat Havlioglu, MD4, Michael Presti, MD5. P1587 - Gastric Intestinal Metaplasia of Duodenum With Subsequent Development of Duodenal Adenoma: An Opportunity for Endoscopic Vigilance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Sayre, PA; 2Saint Mary's Hospital, West Burlington, IA; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4John Cochran VA Medical Center, St. Louis, MO; 5St. Louis Veterans Affairs Medical Center, St. Louis, MO
Introduction: Sporadic non-ampullary duodenal adenomas are detected in patients without familial adenomatous polyposis syndrome with increasing endoscopic visualization. However, progression from duodenal gastric metaplasia remains exceedingly rare with literature
reviews suggesting few case reports.
Case Description/Methods: A 49-year-old female presented with epigastric pain with reported improvement after meals. An EGD for duodenal ulcer evaluation was recommended. Patient had a prior history of chronic GERD with short segment Barrett's without dysplasia diagnosed since 2012, IBS-D and chronic anal fissure. A 5 mm non ampullary lesion was seen in the second portion of duodenum- pathology revealed tubular adenoma with focal high-grade dysplasia, random stomach biopsies were negative for H. pylori. She underwent endoscopic cold snare excision of 5 to 6 mm sessile polyp subsequently on a therapeutic EGD with pathology demonstrating high grade dysplasia arising in tubular adenoma (Figure 1, 2). Prior review of endoscopic evaluations revealed that the patient had undergone an EGD about a year before this presentation for workup of diarrhea, celiac disease and IBS-D. Pathology at that time had showed reactive duodenopathy, duodenal mucosa with gastric mucin metaplasia, Brunner's gland hyperplasia and nonspecific chronic inflammation. There was no dysplasia, acute inflammation, granulomas or villous blunting.
Discussion: Gastric metaplasia of duodenum is most often described in context of H. pylori associated gastritis or NSAID use. Progression to duodenal adenoma is rare with most cases of duodenal gastric metaplasia suggesting endoscopic mucosal defects, inflammation, scar. There remains paucity of surveillance and treatment guidelines for this entity in the absence of H. pylori. The present case highlights the necessity of endoscopic vigilance in patients with gastric metaplasia of duodenum. Given established transformation risk to adenocarcinoma and duodenal adenomas, resection with cold snare or EMR, remains recommended for non- ampullary duodenal lesions. However, there are no current guidelines for subsequent endoscopic surveillance gastric metaplasia of duodenum.
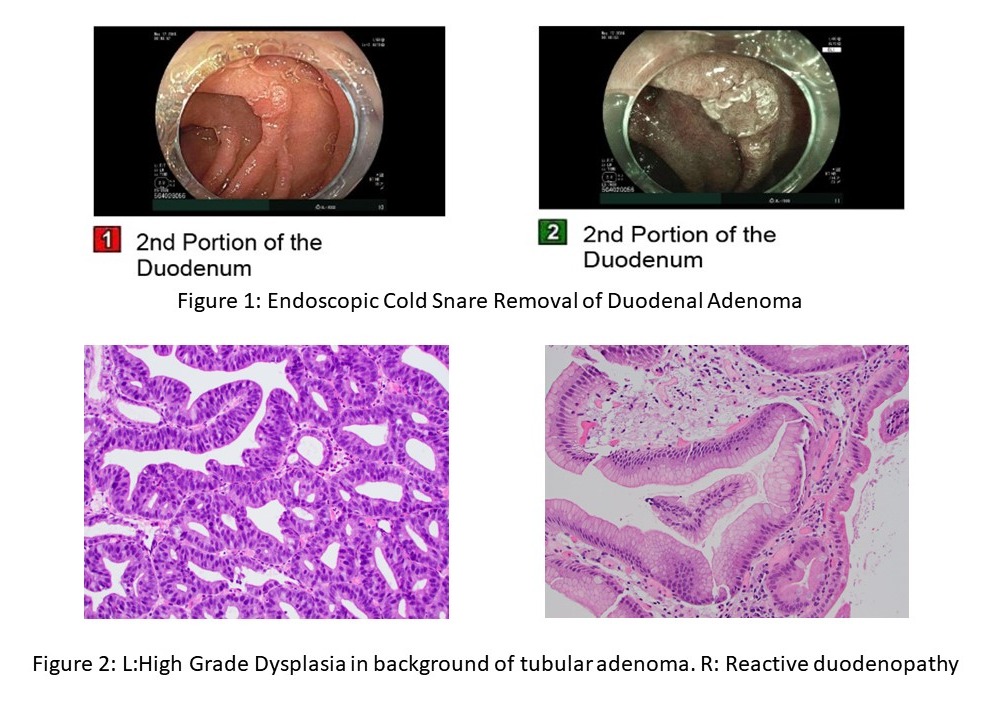
Figure: Figure 1: Endoscopic cold snare excision of duodenal adenoma
Figure 2: L: tubular adenoma with focal high-grade dysplasia. R: reactive duodenopathy, duodenal mucosa with gastric mucin metaplasia, Brunner's gland hyperplasia
Figure 2: L: tubular adenoma with focal high-grade dysplasia. R: reactive duodenopathy, duodenal mucosa with gastric mucin metaplasia, Brunner's gland hyperplasia
Disclosures:
Amlish Gondal indicated no relevant financial relationships.
Aftab Sharif indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Necat Havlioglu indicated no relevant financial relationships.
Michael Presti indicated no relevant financial relationships.
Amlish Gondal, MD1, Aftab Sharif, MD2, Umer Farooq, MD3, Necat Havlioglu, MD4, Michael Presti, MD5. P1587 - Gastric Intestinal Metaplasia of Duodenum With Subsequent Development of Duodenal Adenoma: An Opportunity for Endoscopic Vigilance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
