Sunday Poster Session
Category: Small Intestine
P1591 - Tuberculosis Ileitis Presenting as Small Bowel Obstruction
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NS
Nupur Savalia, MD
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Nupur Savalia, MD1, Joy-Marie Hermes, MD2, Nabil El Hage Chehade, MD3, Faizi Hai, MD1, Andrew Cummins, MD1
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Clinic & Scripps Research Institute, San Diego, CA; 3Scripps Clinic, San Diego, CA
Introduction: Tuberculous ileitis (TB) is a rare occurrence, especially in non-endemic regions and non-immunocompromised patients. However, given increased immigrant populations from high risk regions in the United States, clinical presentations consistent with terminal ileitis warrant careful consideration during initial workup.
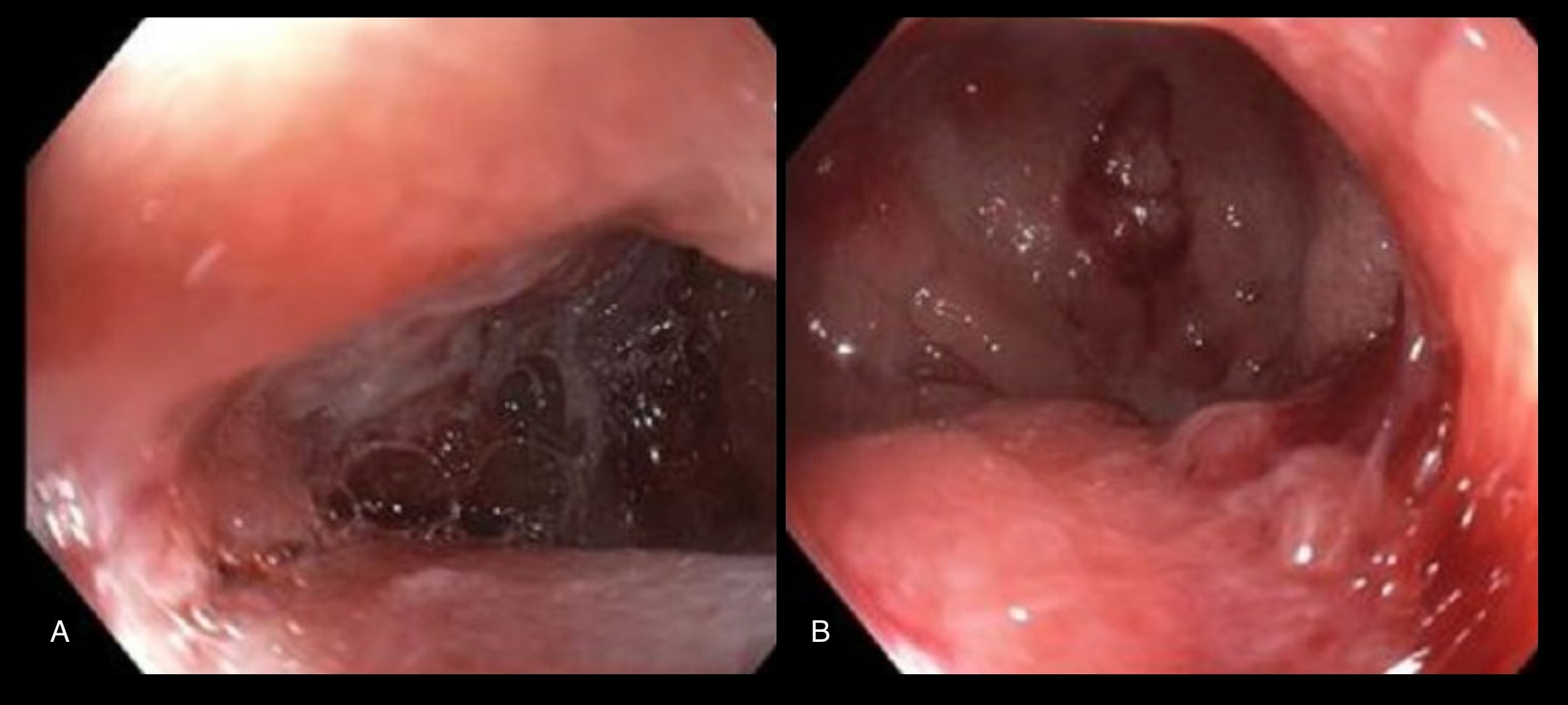
Case Description/Methods: An 18 year old male Ethiopian college student with no significant medical history presented with 1 month of abdominal pain, nausea, decreased appetite, and 27 pound weight loss. On multiple prior emergency department visits, he was diagnosed with enteritis based on imaging and recommended supportive care. CT on presentation showed a high-grade small bowel obstruction (SBO) and mucosal hyperenhancement from the mid jejunum to terminal ileum without a mass or abscess. After nasogastric decompression and initiation of total parenteral nutrition, he underwent colonoscopy which demonstrated a strictured ileocecal valve and distal terminal ileum (TI) with ulceration. Acid fast bacilli (AFB) stain was positive for mycobacteria, suggesting TB ileitis. After initial mild improvement, repeat MRI demonstrated recurrent SBO. He ultimately underwent definitive surgical treatment with right ileocolectomy. Interestingly, intraoperative visualization of the TI demonstrated fat stranding and inflammation, similar to Crohn’s disease. Surgical histopathology demonstrated non-necrotizing granulomas with negative AFB stain. Infectious disease concluded this was likely paucibacillary disease and recommended a six month RIPE regimen.
Discussion: TB ileitis is a rare disease which can mimic other conditions, notably Crohn’s disease (CD). There are reported cases in which patients were misdiagnosed with CD and placed on immunosuppression, ultimately leading to disseminated TB. This case highlights that careful considerations should be taken when postulating a differential diagnosis, including demographic and social factors such as ethnicity, travel from endemic regions, and history of immunosuppression. Tissue biopsy is required for diagnosis however isolated negative biopsies may be reflective of paucibacillary disease in the appropriate clinical context. A multidisciplinary approach to management should be utilized to optimize outcomes. Treatment includes anti-tuberculosis regimens.
Disclosures:
Nupur Savalia, MD1, Joy-Marie Hermes, MD2, Nabil El Hage Chehade, MD3, Faizi Hai, MD1, Andrew Cummins, MD1. P1591 - Tuberculosis Ileitis Presenting as Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Clinic & Scripps Research Institute, San Diego, CA; 3Scripps Clinic, San Diego, CA
Introduction: Tuberculous ileitis (TB) is a rare occurrence, especially in non-endemic regions and non-immunocompromised patients. However, given increased immigrant populations from high risk regions in the United States, clinical presentations consistent with terminal ileitis warrant careful consideration during initial workup.
Case Description/Methods: An 18 year old male Ethiopian college student with no significant medical history presented with 1 month of abdominal pain, nausea, decreased appetite, and 27 pound weight loss. On multiple prior emergency department visits, he was diagnosed with enteritis based on imaging and recommended supportive care. CT on presentation showed a high-grade small bowel obstruction (SBO) and mucosal hyperenhancement from the mid jejunum to terminal ileum without a mass or abscess. After nasogastric decompression and initiation of total parenteral nutrition, he underwent colonoscopy which demonstrated a strictured ileocecal valve and distal terminal ileum (TI) with ulceration. Acid fast bacilli (AFB) stain was positive for mycobacteria, suggesting TB ileitis. After initial mild improvement, repeat MRI demonstrated recurrent SBO. He ultimately underwent definitive surgical treatment with right ileocolectomy. Interestingly, intraoperative visualization of the TI demonstrated fat stranding and inflammation, similar to Crohn’s disease. Surgical histopathology demonstrated non-necrotizing granulomas with negative AFB stain. Infectious disease concluded this was likely paucibacillary disease and recommended a six month RIPE regimen.
Discussion: TB ileitis is a rare disease which can mimic other conditions, notably Crohn’s disease (CD). There are reported cases in which patients were misdiagnosed with CD and placed on immunosuppression, ultimately leading to disseminated TB. This case highlights that careful considerations should be taken when postulating a differential diagnosis, including demographic and social factors such as ethnicity, travel from endemic regions, and history of immunosuppression. Tissue biopsy is required for diagnosis however isolated negative biopsies may be reflective of paucibacillary disease in the appropriate clinical context. A multidisciplinary approach to management should be utilized to optimize outcomes. Treatment includes anti-tuberculosis regimens.
Figure: Stricture and ulceration in the terminal ileum
Disclosures:
Nupur Savalia indicated no relevant financial relationships.
Joy-Marie Hermes indicated no relevant financial relationships.
Nabil El Hage Chehade indicated no relevant financial relationships.
Faizi Hai indicated no relevant financial relationships.
Andrew Cummins indicated no relevant financial relationships.
Nupur Savalia, MD1, Joy-Marie Hermes, MD2, Nabil El Hage Chehade, MD3, Faizi Hai, MD1, Andrew Cummins, MD1. P1591 - Tuberculosis Ileitis Presenting as Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
