Sunday Poster Session
Category: Practice Management
P1517 - Optimizing Resident Consults to GI Service: An Examination in Consults That Result in One Note and Sign Off
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Heng K. Nhoung, MD
Northwell Health
Long Island City, NY
Presenting Author(s)
Heng K. Nhoung, MD1, WonKyung Cho, MD, MPH2, Shivani Sreenivasan, MBBS3, Ji Soo Moon, NP4, Henry Jen, MD5
1Northwell Health, Long Island City, NY; 2Long Island Jewish Medical Center, Forest Hills - Northwell Health, New York, NY; 3Long Island Jewish Medical Center, Forest Hills- Northwell Health, Forest Hills, NY; 4Long Island Jewish Forest Hills, Forest Hills, NY; 5Long Island Jewish Medical Center, Forest Hills - Northwell Health, Forest Hills, NY
Introduction: This quality improvement (QI) project is to identify, evaluate, and reduce the frequency of sub-optimal gastrointestinal (GI) consultations in our healthcare facility. Prior studies looked at consultations deemed inappropriate by the GI service with interventions in education.1,2 This study identifies the number of sub-optimal consults, assess resident knowledge of GI clinical scenarios, and utilizes various tools to decrease sub-optimal consults and increase resident knowledge.
Methods: This study was conducted from 10/2023-04/2024, including GI consult records from Oct-Dec 2023 (pre-intervention), Jan-Feb (intervention) and Mar-Apr (post-intervention). Inclusion Criteria included consultations from internal medicine residents. Exclusion criteria were consults from non-Internal Medicine residents. Sub-optimal consults were defined by one-note signoffs. Resident knowledge was assessed using medical board style questionnaires, pre- and post-intervention. Interventions included a lecture, dispersion of educational materials and utilization of “dot phrases” on our electronic medical records to aid residents in common GI admissions.
Results: No significant differences in one note sign offs were observed pre- and post-interventions. Common one note sign offs included, resolved GI bleeds, no necessity for acute GI interventions and patient refusal (Table 1). There were discrepancies in one note sign offs were noted between hospitalist patients and private attendings. Resident’s report having less freedom in decision making for a consult when working with a private attending. Of note, interventions reduced someone note sign offs in hospitalist patients but had no effect on private attending’s consults. For residents’ knowledge, residents scored better on GI questionnaires post-intervention (p=0.2).
Discussion: Several consults that had one note sign offs from the GI service were GI bleeds that self-resolved. Due to the unpredictability of a GI-bleed these types of consults are likely to continue. Secondly, residents work with both hospitalists and private attendings that may have different viewpoints. This made guideline directed management more challenging. Thirdly, there were patients that refused intervention after their interaction with the GI team. Areas where residents can still improve include; documenting a DRE and determining if patients already have outpatient GI follow up. Future studies can examine factors that lead to resolution of bleeding and streamline consultations to outpatient follow up.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Heng K. Nhoung, MD1, WonKyung Cho, MD, MPH2, Shivani Sreenivasan, MBBS3, Ji Soo Moon, NP4, Henry Jen, MD5. P1517 - Optimizing Resident Consults to GI Service: An Examination in Consults That Result in One Note and Sign Off, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Northwell Health, Long Island City, NY; 2Long Island Jewish Medical Center, Forest Hills - Northwell Health, New York, NY; 3Long Island Jewish Medical Center, Forest Hills- Northwell Health, Forest Hills, NY; 4Long Island Jewish Forest Hills, Forest Hills, NY; 5Long Island Jewish Medical Center, Forest Hills - Northwell Health, Forest Hills, NY
Introduction: This quality improvement (QI) project is to identify, evaluate, and reduce the frequency of sub-optimal gastrointestinal (GI) consultations in our healthcare facility. Prior studies looked at consultations deemed inappropriate by the GI service with interventions in education.1,2 This study identifies the number of sub-optimal consults, assess resident knowledge of GI clinical scenarios, and utilizes various tools to decrease sub-optimal consults and increase resident knowledge.
Methods: This study was conducted from 10/2023-04/2024, including GI consult records from Oct-Dec 2023 (pre-intervention), Jan-Feb (intervention) and Mar-Apr (post-intervention). Inclusion Criteria included consultations from internal medicine residents. Exclusion criteria were consults from non-Internal Medicine residents. Sub-optimal consults were defined by one-note signoffs. Resident knowledge was assessed using medical board style questionnaires, pre- and post-intervention. Interventions included a lecture, dispersion of educational materials and utilization of “dot phrases” on our electronic medical records to aid residents in common GI admissions.
Results: No significant differences in one note sign offs were observed pre- and post-interventions. Common one note sign offs included, resolved GI bleeds, no necessity for acute GI interventions and patient refusal (Table 1). There were discrepancies in one note sign offs were noted between hospitalist patients and private attendings. Resident’s report having less freedom in decision making for a consult when working with a private attending. Of note, interventions reduced someone note sign offs in hospitalist patients but had no effect on private attending’s consults. For residents’ knowledge, residents scored better on GI questionnaires post-intervention (p=0.2).
Discussion: Several consults that had one note sign offs from the GI service were GI bleeds that self-resolved. Due to the unpredictability of a GI-bleed these types of consults are likely to continue. Secondly, residents work with both hospitalists and private attendings that may have different viewpoints. This made guideline directed management more challenging. Thirdly, there were patients that refused intervention after their interaction with the GI team. Areas where residents can still improve include; documenting a DRE and determining if patients already have outpatient GI follow up. Future studies can examine factors that lead to resolution of bleeding and streamline consultations to outpatient follow up.
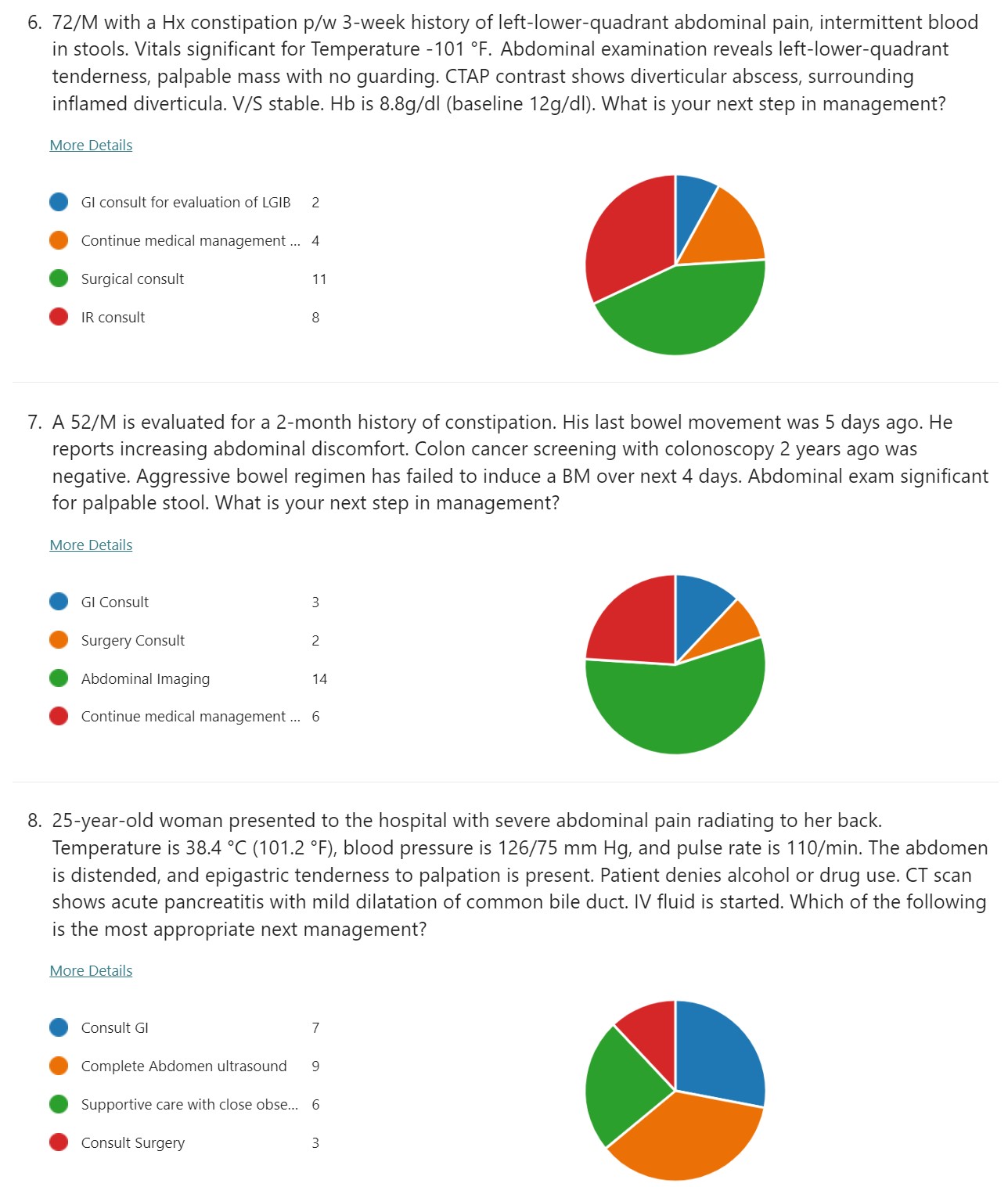
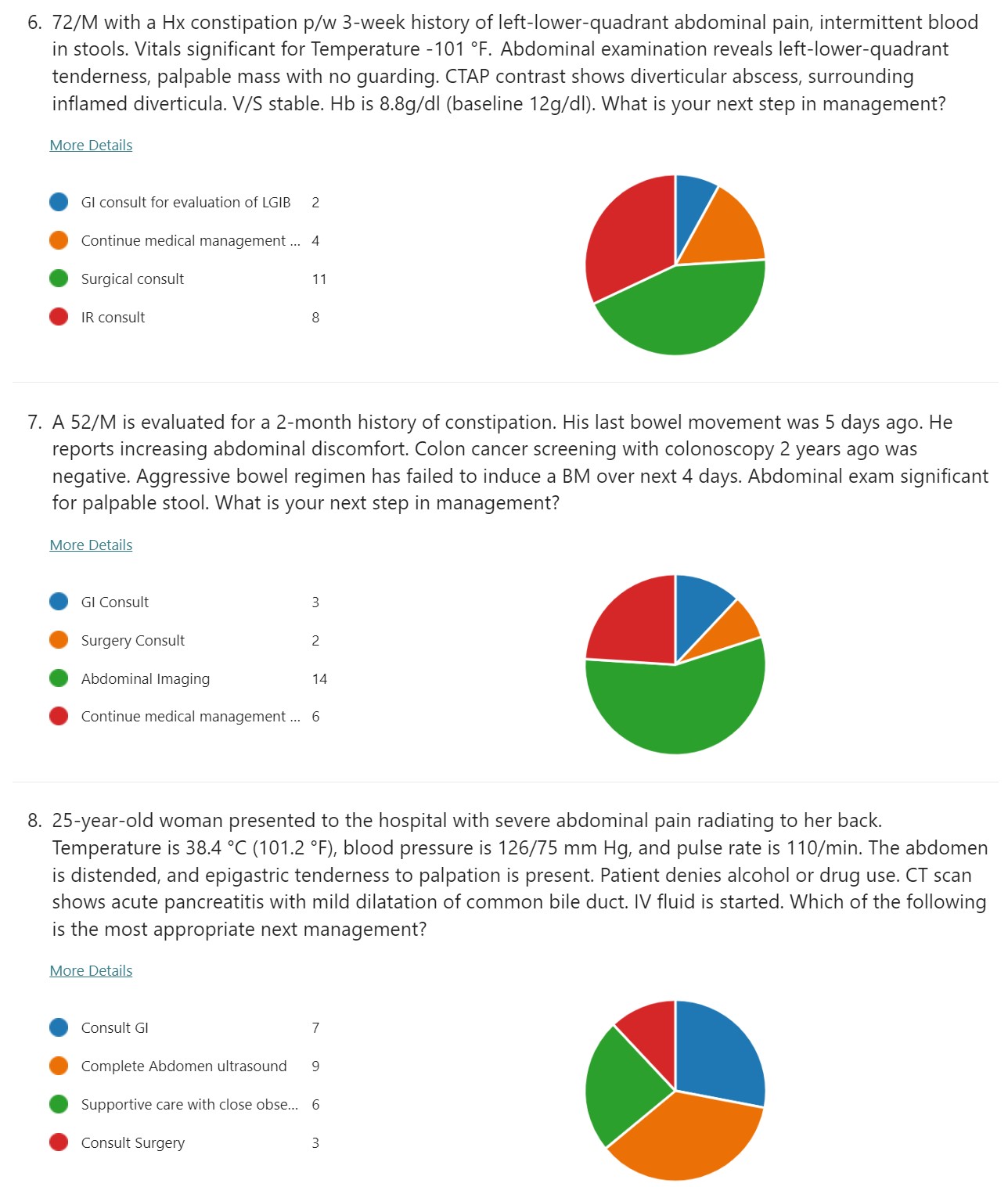
Figure: Example of Resident Assessment Question/Results
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Heng Nhoung indicated no relevant financial relationships.
WonKyung Cho indicated no relevant financial relationships.
Shivani Sreenivasan indicated no relevant financial relationships.
Ji Soo Moon indicated no relevant financial relationships.
Henry Jen indicated no relevant financial relationships.
Heng K. Nhoung, MD1, WonKyung Cho, MD, MPH2, Shivani Sreenivasan, MBBS3, Ji Soo Moon, NP4, Henry Jen, MD5. P1517 - Optimizing Resident Consults to GI Service: An Examination in Consults That Result in One Note and Sign Off, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
