Sunday Poster Session
Category: Small Intestine
P1527 - The Association of Nutritional Status with Mortality in Geriatric Patients With Cancer - A 4.5-Year Prospective Study Using Validated Screening Tools
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sidra Naz, MD, MPH
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Sidra Naz, MD, MPH1, Juhee Song, PhD2, Irene J. Lee, MD3, Muhammad Ali Khan, MD4, Anam Khan, MD2, Mehnaz A. Shafi, MD1
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3Baylor College of Medicine, Houston, TX; 4MD Anderson Cancer Center, Houston, TX
Introduction: Malnutrition in the elderly is under-recognized yet common, affecting 25-60% of geriatric care facilities and 35-65% of hospitalized adults. It is linked to higher mortality, lower quality of life, poor treatment response, and increased chemotherapy toxicity. Its impact on geriatric cancer patients is less well-known.
Methods: We studied the association between nutritional status (assessed by MNA, weight loss, BMI, and lean muscle mass) and 6- and 12-month mortality in geriatric cancer patients,
adjusting for covariates. From 2019-2023, we prospectively included patients over 65 with
malignancies who completed initial and 6-month follow-up nutritional assessments. Univariate Cox regression assessed the link between nutritional status and mortality, while logistic regression evaluated 6- and 12-month mortality. Data analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC)
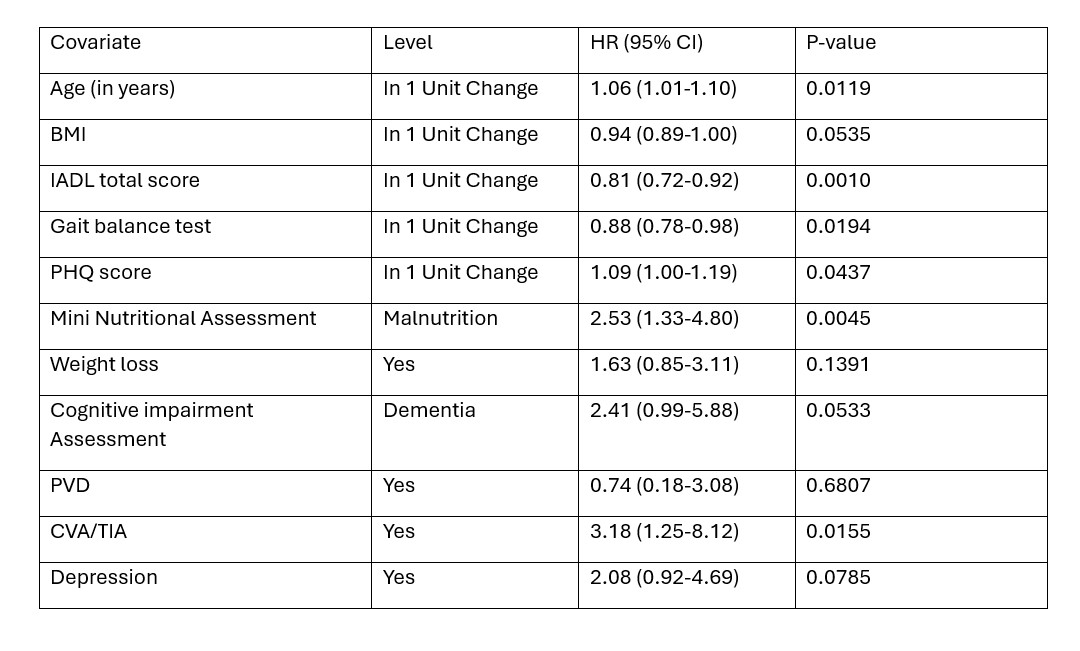
Results: 130 patients met the inclusion criteria, 67 were men (51.5%), with a median age of 74 years, and 86.9% were white. The median follow-up was 55.4 months (reverse Kaplan-Meier method). During follow-up, 41 patients died, and 89 were alive at their last visit. Solid malignancies were present in 76%, primarily GI (19.2%) and hematologic (23.8%), with 43.3% at stage 3-4. Higher mortality risk was statistically associated with older age, lower independent activities of daily living (IADL) total score, poor gait balance, higher Patient Health Questionnaire (PHQ) score, malnutrition, and history of cerebral vascular accident/transient ischemic attack CVA/TIA. Peripheral vascular disease (PVD), CVA/TIA, and dementia increased the odds of 6-month mortality, while lower IADL scores and depression raised 12-month mortality odds
Discussion: Malnutrition is common among the elderly and cancer patients. Long-term data on its impact on survival in cancer patients is limited. Factors associated with higher mortality risk included older age, poor gait balance, and a history of CVA/TIA. This knowledge is crucial for comprehensive care planning and risk reduction in geriatric cancer patients
Disclosures:
Sidra Naz, MD, MPH1, Juhee Song, PhD2, Irene J. Lee, MD3, Muhammad Ali Khan, MD4, Anam Khan, MD2, Mehnaz A. Shafi, MD1. P1527 - The Association of Nutritional Status with Mortality in Geriatric Patients With Cancer - A 4.5-Year Prospective Study Using Validated Screening Tools, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3Baylor College of Medicine, Houston, TX; 4MD Anderson Cancer Center, Houston, TX
Introduction: Malnutrition in the elderly is under-recognized yet common, affecting 25-60% of geriatric care facilities and 35-65% of hospitalized adults. It is linked to higher mortality, lower quality of life, poor treatment response, and increased chemotherapy toxicity. Its impact on geriatric cancer patients is less well-known.
Methods: We studied the association between nutritional status (assessed by MNA, weight loss, BMI, and lean muscle mass) and 6- and 12-month mortality in geriatric cancer patients,
adjusting for covariates. From 2019-2023, we prospectively included patients over 65 with
malignancies who completed initial and 6-month follow-up nutritional assessments. Univariate Cox regression assessed the link between nutritional status and mortality, while logistic regression evaluated 6- and 12-month mortality. Data analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC)
Results: 130 patients met the inclusion criteria, 67 were men (51.5%), with a median age of 74 years, and 86.9% were white. The median follow-up was 55.4 months (reverse Kaplan-Meier method). During follow-up, 41 patients died, and 89 were alive at their last visit. Solid malignancies were present in 76%, primarily GI (19.2%) and hematologic (23.8%), with 43.3% at stage 3-4. Higher mortality risk was statistically associated with older age, lower independent activities of daily living (IADL) total score, poor gait balance, higher Patient Health Questionnaire (PHQ) score, malnutrition, and history of cerebral vascular accident/transient ischemic attack CVA/TIA. Peripheral vascular disease (PVD), CVA/TIA, and dementia increased the odds of 6-month mortality, while lower IADL scores and depression raised 12-month mortality odds
Discussion: Malnutrition is common among the elderly and cancer patients. Long-term data on its impact on survival in cancer patients is limited. Factors associated with higher mortality risk included older age, poor gait balance, and a history of CVA/TIA. This knowledge is crucial for comprehensive care planning and risk reduction in geriatric cancer patients
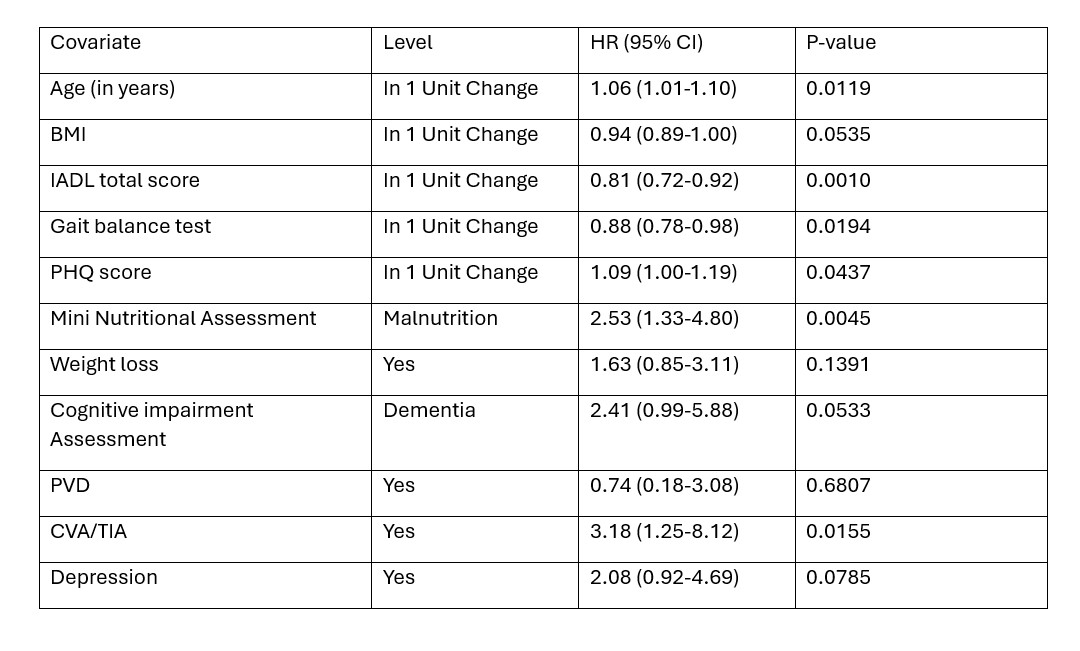
Figure: Table:1 Univariate Cox regression on overall survival since CGA evaluation: BMI: Body mass index, IADL: Independent activities of daily living, MOCA: Montreal Cognitive Assessment, PHQ: Patient Health Questionnaire, PVD: Peripheral vascular disease, CVA: cerebral vascular accident, TIA: Transient ischemic attack
Disclosures:
Sidra Naz indicated no relevant financial relationships.
Juhee Song indicated no relevant financial relationships.
Irene Lee indicated no relevant financial relationships.
Muhammad Ali Khan indicated no relevant financial relationships.
Anam Khan indicated no relevant financial relationships.
Mehnaz Shafi indicated no relevant financial relationships.
Sidra Naz, MD, MPH1, Juhee Song, PhD2, Irene J. Lee, MD3, Muhammad Ali Khan, MD4, Anam Khan, MD2, Mehnaz A. Shafi, MD1. P1527 - The Association of Nutritional Status with Mortality in Geriatric Patients With Cancer - A 4.5-Year Prospective Study Using Validated Screening Tools, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
