Sunday Poster Session
Category: Liver
P1430 - A Subhepatic Abscess Due to Dropped Gallstone Diagnosed in the Outpatient Gastroenterology Clinic
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Danzhu Zhao, DO
University of Connecticut Health Center
WEST HARTFORD, CT
Presenting Author(s)
Danzhu Zhao, DO1, Neil Khoury, MD2, Roopjeet K. Bath, MBBS3
1University of Connecticut Health Center, Farmington, CT; 2UConn Health, Hartford, CT; 3UConn Health, Farmington, CT
Introduction: Spilled gallstones during a laparoscopic cholecystectomy (LC) is a common complication that rarely manifests weeks to years later as an abscess. We present a patient who developed a subhepatic abscess 4 years after his LC who presented without classic signs of infection.
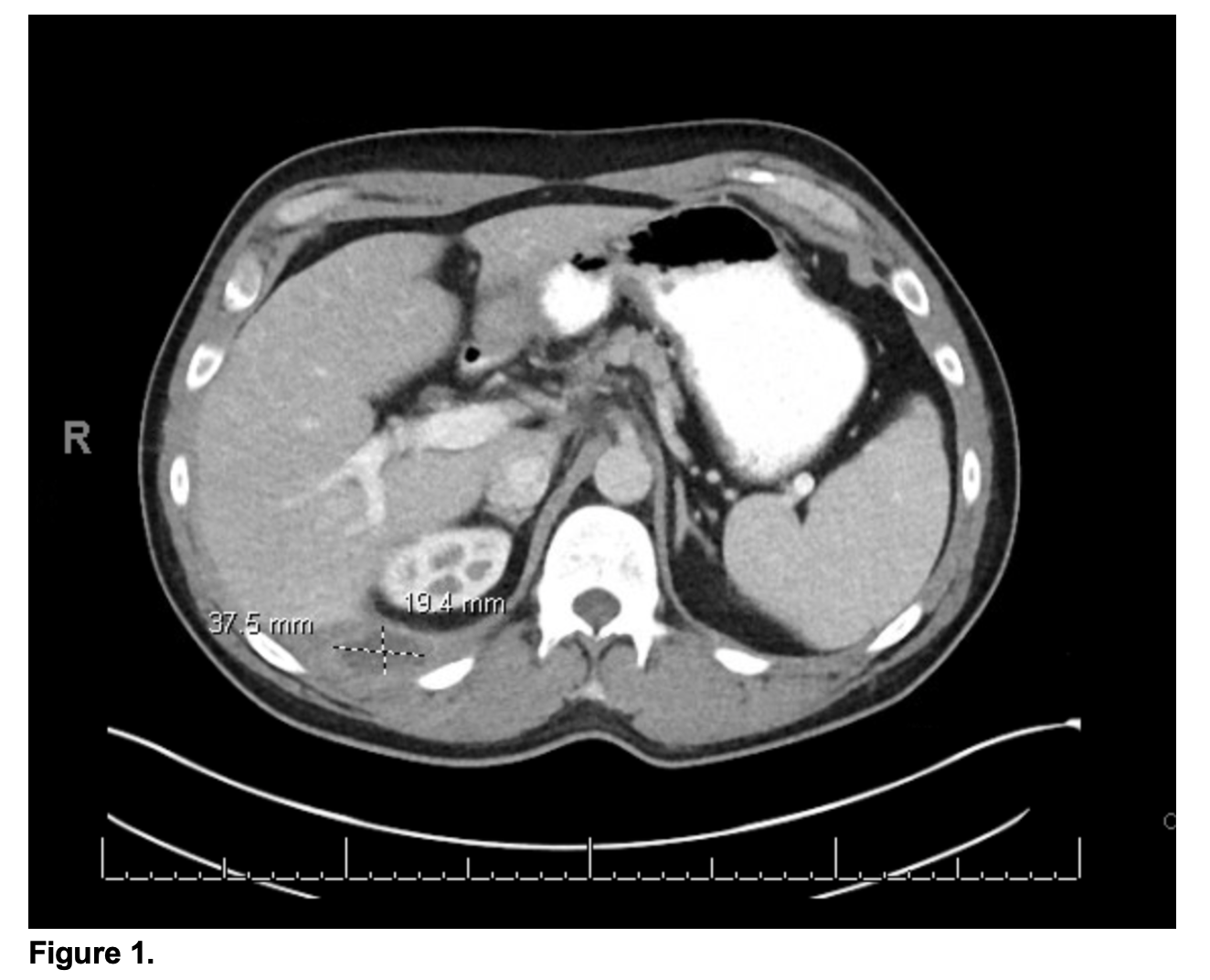
Case Description/Methods: A 47-year-old male with surgical history of LC for biliary colic 4 years prior presented to the GI clinic with abdominal pain. Vitals were unremarkable. His abdomen was soft and without tenderness. His blood work revealed normal liver panel including AST, ALT, ALP and T bilirubin without leukocytosis. Abdominal ultrasound revealed 4.4 cm x 2.8 cm x 2.2 cm heterogeneously hypoechoic fluid along the posterior aspect of the right lobe of the liver with punctate peripheral echogenic foci along the margins. Abdominal CT with contrast showed a few small hepatic hypodensities and a rim-enhancing fluid collection abutting the posterior margin of the right hepatic lobe concerning for an abscess due to a dropped gallstone (Figure 1). A pigtail drain was placed by interventional radiology with purulent drainage. Fluid culture grew Klebsiella and Enterococcus and the patient was treated with a 7-day course of Amoxicillin/Clavulanic acid. Repeat abdominal CT showed resolution of the abscess and the previously suspected dropped gallstones were no longer visualized. The drain was successfully removed 1 week later. The patient’s abdominal pain resolved.
Discussion: Gallstone spillage is a common intraoperative complication during LCs which can rarely become a nidus for infection and abscess formation. Gallstone abscesses can be difficult to diagnose as they may form weeks to years after LC. Patients often present with signs of infection such as fevers and leukocytosis, along with abdominal pain, nausea and vomiting, and typically seek attention in an emergency room. Our patient had a mild, nonspecific presentation with vague abdominal symptoms without any signs of infection, and he was diagnosed as an outpatient. Similar cases will require a high index of suspicion for prompt diagnosis. Abdominal US and contrast enhanced CT imaging are diagnostic tools that will localize an abscess and a corresponding radio-opaque gallstone, though radio-lucent gallstones can be easily missed on imaging. The mainstay of management is antibiotics plus aspiration, drain placement, or intraoperative drainage, depending on the abscess size and location.
Disclosures:
Danzhu Zhao, DO1, Neil Khoury, MD2, Roopjeet K. Bath, MBBS3. P1430 - A Subhepatic Abscess Due to Dropped Gallstone Diagnosed in the Outpatient Gastroenterology Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2UConn Health, Hartford, CT; 3UConn Health, Farmington, CT
Introduction: Spilled gallstones during a laparoscopic cholecystectomy (LC) is a common complication that rarely manifests weeks to years later as an abscess. We present a patient who developed a subhepatic abscess 4 years after his LC who presented without classic signs of infection.
Case Description/Methods: A 47-year-old male with surgical history of LC for biliary colic 4 years prior presented to the GI clinic with abdominal pain. Vitals were unremarkable. His abdomen was soft and without tenderness. His blood work revealed normal liver panel including AST, ALT, ALP and T bilirubin without leukocytosis. Abdominal ultrasound revealed 4.4 cm x 2.8 cm x 2.2 cm heterogeneously hypoechoic fluid along the posterior aspect of the right lobe of the liver with punctate peripheral echogenic foci along the margins. Abdominal CT with contrast showed a few small hepatic hypodensities and a rim-enhancing fluid collection abutting the posterior margin of the right hepatic lobe concerning for an abscess due to a dropped gallstone (Figure 1). A pigtail drain was placed by interventional radiology with purulent drainage. Fluid culture grew Klebsiella and Enterococcus and the patient was treated with a 7-day course of Amoxicillin/Clavulanic acid. Repeat abdominal CT showed resolution of the abscess and the previously suspected dropped gallstones were no longer visualized. The drain was successfully removed 1 week later. The patient’s abdominal pain resolved.
Discussion: Gallstone spillage is a common intraoperative complication during LCs which can rarely become a nidus for infection and abscess formation. Gallstone abscesses can be difficult to diagnose as they may form weeks to years after LC. Patients often present with signs of infection such as fevers and leukocytosis, along with abdominal pain, nausea and vomiting, and typically seek attention in an emergency room. Our patient had a mild, nonspecific presentation with vague abdominal symptoms without any signs of infection, and he was diagnosed as an outpatient. Similar cases will require a high index of suspicion for prompt diagnosis. Abdominal US and contrast enhanced CT imaging are diagnostic tools that will localize an abscess and a corresponding radio-opaque gallstone, though radio-lucent gallstones can be easily missed on imaging. The mainstay of management is antibiotics plus aspiration, drain placement, or intraoperative drainage, depending on the abscess size and location.
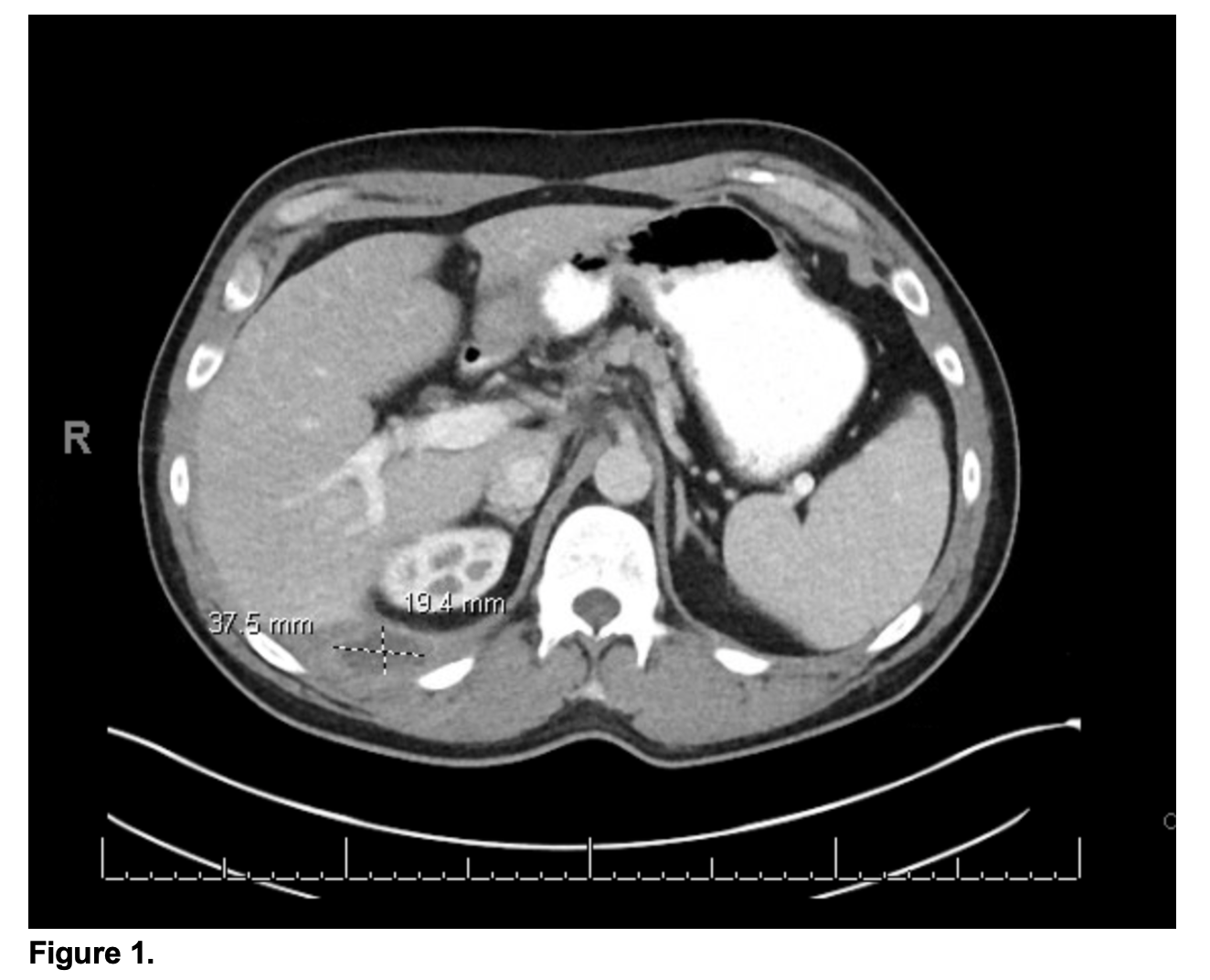
Figure: Figure 1. Rim-enhancing fluid collection abutting the posterior margin of the right hepatic lobe.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Neil Khoury indicated no relevant financial relationships.
Roopjeet Bath indicated no relevant financial relationships.
Danzhu Zhao, DO1, Neil Khoury, MD2, Roopjeet K. Bath, MBBS3. P1430 - A Subhepatic Abscess Due to Dropped Gallstone Diagnosed in the Outpatient Gastroenterology Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
