Sunday Poster Session
Category: Liver
P1434 - An Atypical Case of Ketamine-Induced Hepatocellular Liver Injury
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kevin R. O'Connor, MD
California Pacific Medical Center
San Francisco, CA
Presenting Author(s)
Kevin R. O'Connor, MD1, Ingeborg Schafhalter-Zoppoth, MD2
1California Pacific Medical Center, San Francisco, CA; 2Sutter West Bay Medical Group, San Francisco, CA
Introduction: Ketamine is a dissociative anesthetic with evidence supporting off-label use in subanesthetic doses to treat pain and mood disorders. These applications have contributed to growing clinician interest and public recreational use. Well-known adverse effects of ketamine include hypertension/tachycardia, respiratory depression, and ulcerative cystitis. As its prevalence increases, evidence of lesser-known effects is emerging including liver injury.
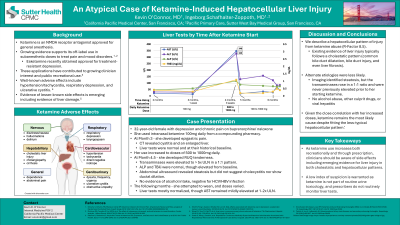
Case Description/Methods: A 32-year-old female with depression and chronic pain on buprenorphine/naloxone treated her conditions with intranasal ketamine 100 mg daily from a compounding pharmacy. At Month 3 of her use, she developed epigastric pain and a CT revealed cystitis; LFTs were normal and at their historical baseline. Soon after, she increased daily ingestion to 500 to 1000 mg daily (IN and PO). At Month 4.5, she developed RUQ tenderness. Her transaminases were elevated to greater than five times ULN in a 1:1 pattern with alkaline phosphatase and total bilirubin normal, though elevated from baseline. Abdominal ultrasound revealed steatosis but did not suggest cholecystitis nor show ductal dilation. She denied alcohol intake, confirmed by labs, which were also negative for HCV/HBV infection. She attempted to wean her ketamine the following month and doses varied. Her LFTs mostly normalized, though AST remained mildly elevated at one to two times ULN.
Discussion: Increasing evidence ties ketamine abuse to liver injury, however, most of these cases follow a cholestatic pattern. It has been linked to common bile duct dilatation, bile duct injury, and even liver fibrosis. We describe a hepatocellular pattern of injury from ketamine abuse. While our patient’s alkaline phosphatase and total bilirubin did rise to nearly three times their baseline values from the months prior, each was still within the upper limits of normal, and the R-Factor was 8.5. Alternate etiologies were less likely. Imaging identified steatosis, but the transaminases rose in a 1:1 ratio and were never previously elevated prior to her starting ketamine. Further, there was no evidence of alcohol abuse or viral hepatitis. Given the close correlation with her increased doses, ketamine remains the most likely cause despite fitting the less-typical hepatocellular pattern.
As ketamine use increases both recreationally and through prescription, clinicians should be aware of side effects including emerging evidence for liver injury in both cholestatic and hepatocellular patterns.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kevin R. O'Connor, MD1, Ingeborg Schafhalter-Zoppoth, MD2. P1434 - An Atypical Case of Ketamine-Induced Hepatocellular Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1California Pacific Medical Center, San Francisco, CA; 2Sutter West Bay Medical Group, San Francisco, CA
Introduction: Ketamine is a dissociative anesthetic with evidence supporting off-label use in subanesthetic doses to treat pain and mood disorders. These applications have contributed to growing clinician interest and public recreational use. Well-known adverse effects of ketamine include hypertension/tachycardia, respiratory depression, and ulcerative cystitis. As its prevalence increases, evidence of lesser-known effects is emerging including liver injury.
Case Description/Methods: A 32-year-old female with depression and chronic pain on buprenorphine/naloxone treated her conditions with intranasal ketamine 100 mg daily from a compounding pharmacy. At Month 3 of her use, she developed epigastric pain and a CT revealed cystitis; LFTs were normal and at their historical baseline. Soon after, she increased daily ingestion to 500 to 1000 mg daily (IN and PO). At Month 4.5, she developed RUQ tenderness. Her transaminases were elevated to greater than five times ULN in a 1:1 pattern with alkaline phosphatase and total bilirubin normal, though elevated from baseline. Abdominal ultrasound revealed steatosis but did not suggest cholecystitis nor show ductal dilation. She denied alcohol intake, confirmed by labs, which were also negative for HCV/HBV infection. She attempted to wean her ketamine the following month and doses varied. Her LFTs mostly normalized, though AST remained mildly elevated at one to two times ULN.
Discussion: Increasing evidence ties ketamine abuse to liver injury, however, most of these cases follow a cholestatic pattern. It has been linked to common bile duct dilatation, bile duct injury, and even liver fibrosis. We describe a hepatocellular pattern of injury from ketamine abuse. While our patient’s alkaline phosphatase and total bilirubin did rise to nearly three times their baseline values from the months prior, each was still within the upper limits of normal, and the R-Factor was 8.5. Alternate etiologies were less likely. Imaging identified steatosis, but the transaminases rose in a 1:1 ratio and were never previously elevated prior to her starting ketamine. Further, there was no evidence of alcohol abuse or viral hepatitis. Given the close correlation with her increased doses, ketamine remains the most likely cause despite fitting the less-typical hepatocellular pattern.
As ketamine use increases both recreationally and through prescription, clinicians should be aware of side effects including emerging evidence for liver injury in both cholestatic and hepatocellular patterns.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kevin O'Connor indicated no relevant financial relationships.
Ingeborg Schafhalter-Zoppoth indicated no relevant financial relationships.
Kevin R. O'Connor, MD1, Ingeborg Schafhalter-Zoppoth, MD2. P1434 - An Atypical Case of Ketamine-Induced Hepatocellular Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

