Sunday Poster Session
Category: Liver
P1298 - De Novo HBV Infection in a Liver Transplant Recipient Necessitating Re-Transplantation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KJ
Kevan Josloff, MD, MPH
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Kevan Josloff, MD, MPH1, Benjamin Young, MD1, Marc Hersh, MD1, Alekya Bheemreddy, BA2, Sherry Lee, MD, PhD1, Dina Halegoua-DeMarzio, MD2
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Hepatitis B virus (HBV) is the leading cause of cirrhosis worldwide, most commonly due to cases of vertical transmission or infection at a very young age. The risk of acute HBV in adults is higher in immunocompromised patients and is associated with a more rapid progression to chronic HBV infection. However, even in immunocompromised patients, acute HBV infection rarely leads to cirrhosis. We present a case of de-novo HBV infection leading to HBV-related cirrhosis in a 47-year-old liver transplant recipient, necessitating re-transplantation.
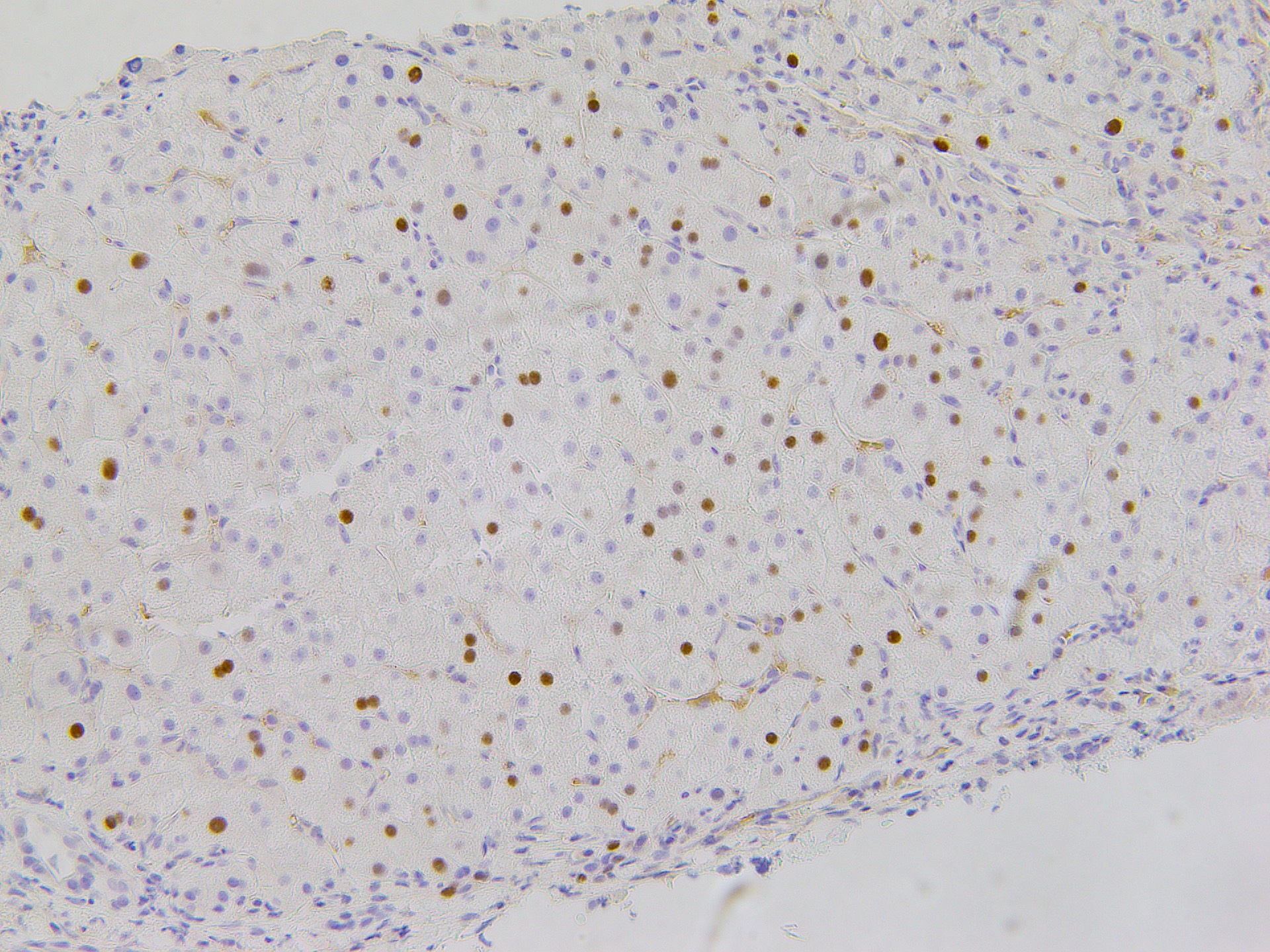
Case Description/Methods: The patient was originally transplanted for a diagnosis of cryptogenic cirrhosis. At the time of transplantation both the donor and recipient were HBsAg, HBsAb, and anti-HBcAb negative. The post-transplant course was complicated by 4 separate instances of acute cellular rejection (RAI 4-5). The patient re-presented to our center 5 years post-transplant with elevated liver enzymes, and subsequently was found to have a new HBV viremia of 16 million copies. Surveillance HBV studies had most recently been negative 3 years before the current presentation, after which no further HBV studies were obtained. Liver biopsy showed stage 4/4 cirrhosis with immunohistochemical staining showing HBcAg positive active HBV cirrhosis as the underlying etiology (Figure 1). The patient underwent re-transplantation two weeks after his initial presentation due to rapid and severe deterioration of liver function. Of note, Hepatitis B immunoglobulin (HBIG) was given peri-transplant.
Discussion: HBV-related cirrhosis typically occurs when a child is infected at a very young age, while HBV contracted as an adult will rarely lead to cirrhosis. HBV vaccination is typically a highly effective preventive measure, although rates of response are notably lower in those with chronic liver disease. In a recent large-scale retrospective study of 2,686 liver transplant patients, 32 patients (1.2%) were found to have a de-novo HBV infection, none of whom progressed to cirrhosis. Multiple studies have found evidence of HBV cirrhosis in post liver transplant patients, however in each instance there was evidence of the donor or the recipient being HBV positive prior to transplantation. Patients with post-transplant HBV infection consistently have worse morbidity and mortality compared to their cohorts. This case report represents a rare manifestation of de-novo HBV-related cirrhosis, and highlights the importance of close follow up in this patient population.
Disclosures:
Kevan Josloff, MD, MPH1, Benjamin Young, MD1, Marc Hersh, MD1, Alekya Bheemreddy, BA2, Sherry Lee, MD, PhD1, Dina Halegoua-DeMarzio, MD2. P1298 - De Novo HBV Infection in a Liver Transplant Recipient Necessitating Re-Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Hepatitis B virus (HBV) is the leading cause of cirrhosis worldwide, most commonly due to cases of vertical transmission or infection at a very young age. The risk of acute HBV in adults is higher in immunocompromised patients and is associated with a more rapid progression to chronic HBV infection. However, even in immunocompromised patients, acute HBV infection rarely leads to cirrhosis. We present a case of de-novo HBV infection leading to HBV-related cirrhosis in a 47-year-old liver transplant recipient, necessitating re-transplantation.
Case Description/Methods: The patient was originally transplanted for a diagnosis of cryptogenic cirrhosis. At the time of transplantation both the donor and recipient were HBsAg, HBsAb, and anti-HBcAb negative. The post-transplant course was complicated by 4 separate instances of acute cellular rejection (RAI 4-5). The patient re-presented to our center 5 years post-transplant with elevated liver enzymes, and subsequently was found to have a new HBV viremia of 16 million copies. Surveillance HBV studies had most recently been negative 3 years before the current presentation, after which no further HBV studies were obtained. Liver biopsy showed stage 4/4 cirrhosis with immunohistochemical staining showing HBcAg positive active HBV cirrhosis as the underlying etiology (Figure 1). The patient underwent re-transplantation two weeks after his initial presentation due to rapid and severe deterioration of liver function. Of note, Hepatitis B immunoglobulin (HBIG) was given peri-transplant.
Discussion: HBV-related cirrhosis typically occurs when a child is infected at a very young age, while HBV contracted as an adult will rarely lead to cirrhosis. HBV vaccination is typically a highly effective preventive measure, although rates of response are notably lower in those with chronic liver disease. In a recent large-scale retrospective study of 2,686 liver transplant patients, 32 patients (1.2%) were found to have a de-novo HBV infection, none of whom progressed to cirrhosis. Multiple studies have found evidence of HBV cirrhosis in post liver transplant patients, however in each instance there was evidence of the donor or the recipient being HBV positive prior to transplantation. Patients with post-transplant HBV infection consistently have worse morbidity and mortality compared to their cohorts. This case report represents a rare manifestation of de-novo HBV-related cirrhosis, and highlights the importance of close follow up in this patient population.
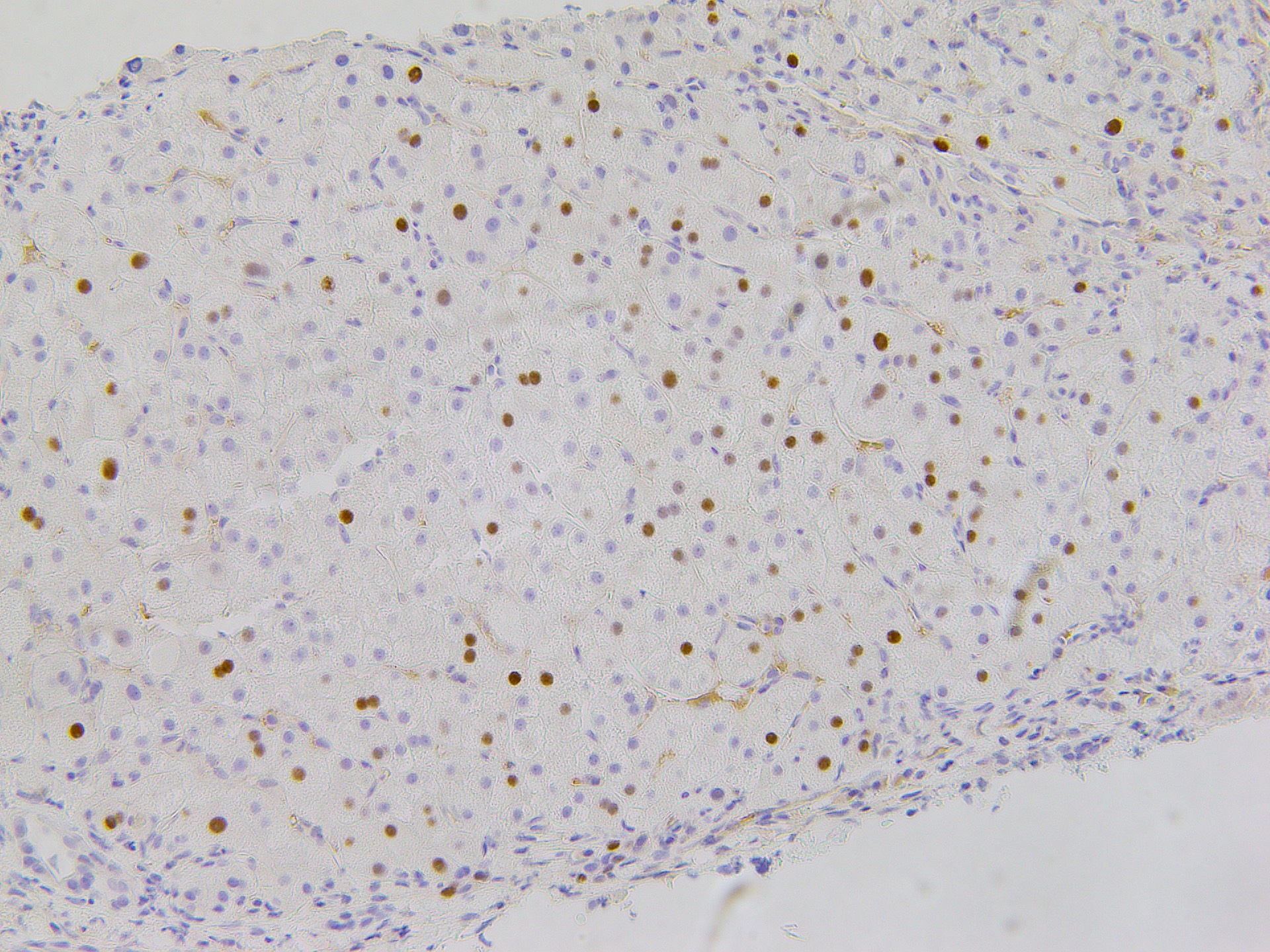
Figure: Figure 1. Liver biopsy stained for HBcAg, showing widespread active HBV infection as the underlying etiology of cirrhosis.
Disclosures:
Kevan Josloff indicated no relevant financial relationships.
Benjamin Young indicated no relevant financial relationships.
Marc Hersh indicated no relevant financial relationships.
Alekya Bheemreddy indicated no relevant financial relationships.
Sherry Lee indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisor or Review Panel Member, Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member, Grant/Research Support. Viking – Grant/Research Support.
Kevan Josloff, MD, MPH1, Benjamin Young, MD1, Marc Hersh, MD1, Alekya Bheemreddy, BA2, Sherry Lee, MD, PhD1, Dina Halegoua-DeMarzio, MD2. P1298 - De Novo HBV Infection in a Liver Transplant Recipient Necessitating Re-Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

