Sunday Poster Session
Category: Liver
P1240 - Intersectional Outcomes in Autoimmune Hepatitis: A Five-Year Cross-Sectional Study, Using NIS, on the Interplay of Gender and Race in AIH and Co-Occurring Rheumatoid Arthritis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sreeram Pannala, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: It’s been reported that there could be a strong association between certain Autoimmune liver diseases and Systemic Rheumatological Diseases. For ex, Autoimmune Hepatitis (AIH) with Sjogren’s, Rheumatoid Arthritis (RA) or Systemic Lupus Erythematosus, as well as Primary Biliary Cirrhosis with Sjogren’s, RA, or Systemic Sclerosis. Moreover, various population analyses showed a 1.6% to 5.4% prevalence of RA in patients with AIH. Our study aims to analyze this clinically significant association and its impact on hepatic complications in hospitalized patients.
Methods: We gathered in-patient data on AIH and RA using the National Inpatient Sample database from 2016 to 2020. We included patients older than 18 years of both genders, admitted with a primary and a secondary diagnosis of RA and AIH. We excluded patients admitted with causes that can alter liver function such as alcohol liver disease, liver transplant, NASH, PBC, PSC, etc. We compared both cohorts, outlined baseline characteristics, & analyzed outcomes such as cirrhosis, HCC, ascites, and upper GI bleed (UGIB), using STATA. We stratified them for gender, race, and comorbidity burden.
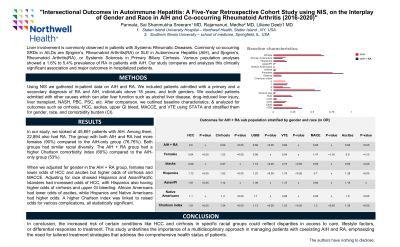
Results: In both cohorts, most patients were white. The AIH + RA cohort had a significant female predominance reaching 90% vs 76.76% in the AIH group. Gender-adjusted analysis in the AIH + RA cohort showed females had lower odds of HCC (OR 0.64, p< 0.002) and ascites (OR 0.9, p< 0.013), but higher odds for cirrhosis (OR 1.12, p< 0.00). Race adjustments revealed Hispanics and Asians with increased odds of HCC (OR 1.73, p< 0.003; OR 1.91, p< 0.011); Hispanics with higher odds for cirrhosis (OR 1.52, p< 0.00), and UGIB (OR 1.23, p< 0.02). Blacks had lower odds of ascites (OR 0.85, p< 0.008), while in Hispanics it was higher (OR 1.28; p< 0.05). Higher Charlson index linked to raised odds for HCC (OR 1.5), cirrhosis (OR 1.34), UGIB (OR 1.14), and ascites (OR 1.29), all statistically significant (p< 0.05).
Discussion: Our study reveals significant disparities in AIH + RA outcomes across racial and gender lines, with notable differences in disease prevalence and complications. Women and certain racial groups exhibit distinct patterns of risk for major hepatic complications like HCC, cirrhosis, and ascites. These findings underscore and warrant further investigation for tailored approaches in managing AIH and RA, highlighting the importance of considering gender and racial backgrounds in clinical strategies to optimize patient care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1. P1240 - Intersectional Outcomes in Autoimmune Hepatitis: A Five-Year Cross-Sectional Study, Using NIS, on the Interplay of Gender and Race in AIH and Co-Occurring Rheumatoid Arthritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Southern Illinois University, Springfield, IL
Introduction: It’s been reported that there could be a strong association between certain Autoimmune liver diseases and Systemic Rheumatological Diseases. For ex, Autoimmune Hepatitis (AIH) with Sjogren’s, Rheumatoid Arthritis (RA) or Systemic Lupus Erythematosus, as well as Primary Biliary Cirrhosis with Sjogren’s, RA, or Systemic Sclerosis. Moreover, various population analyses showed a 1.6% to 5.4% prevalence of RA in patients with AIH. Our study aims to analyze this clinically significant association and its impact on hepatic complications in hospitalized patients.
Methods: We gathered in-patient data on AIH and RA using the National Inpatient Sample database from 2016 to 2020. We included patients older than 18 years of both genders, admitted with a primary and a secondary diagnosis of RA and AIH. We excluded patients admitted with causes that can alter liver function such as alcohol liver disease, liver transplant, NASH, PBC, PSC, etc. We compared both cohorts, outlined baseline characteristics, & analyzed outcomes such as cirrhosis, HCC, ascites, and upper GI bleed (UGIB), using STATA. We stratified them for gender, race, and comorbidity burden.
Results: In both cohorts, most patients were white. The AIH + RA cohort had a significant female predominance reaching 90% vs 76.76% in the AIH group. Gender-adjusted analysis in the AIH + RA cohort showed females had lower odds of HCC (OR 0.64, p< 0.002) and ascites (OR 0.9, p< 0.013), but higher odds for cirrhosis (OR 1.12, p< 0.00). Race adjustments revealed Hispanics and Asians with increased odds of HCC (OR 1.73, p< 0.003; OR 1.91, p< 0.011); Hispanics with higher odds for cirrhosis (OR 1.52, p< 0.00), and UGIB (OR 1.23, p< 0.02). Blacks had lower odds of ascites (OR 0.85, p< 0.008), while in Hispanics it was higher (OR 1.28; p< 0.05). Higher Charlson index linked to raised odds for HCC (OR 1.5), cirrhosis (OR 1.34), UGIB (OR 1.14), and ascites (OR 1.29), all statistically significant (p< 0.05).
Discussion: Our study reveals significant disparities in AIH + RA outcomes across racial and gender lines, with notable differences in disease prevalence and complications. Women and certain racial groups exhibit distinct patterns of risk for major hepatic complications like HCC, cirrhosis, and ascites. These findings underscore and warrant further investigation for tailored approaches in managing AIH and RA, highlighting the importance of considering gender and racial backgrounds in clinical strategies to optimize patient care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Medha Rajamanuri indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala, MD1, Medha Rajamanuri, MBBS2, Liliane Deeb, MD1. P1240 - Intersectional Outcomes in Autoimmune Hepatitis: A Five-Year Cross-Sectional Study, Using NIS, on the Interplay of Gender and Race in AIH and Co-Occurring Rheumatoid Arthritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
