Sunday Poster Session
Category: Liver
P1241 - Improving Adherence to Quality Metrics in Cirrhosis Care at a Tertiary Care Center: A Quality Improvement Project
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Alexander Garcia, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Alexander Garcia, DO1, Avneet Singh, DO1, Mahir Qureshi, MD1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Kathy N. Williams, MD, MS4, Jason Ho, MD5, Christopher Deitch, MD5
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Health Care, Camden, NJ; 4Cooper University Hospital, Philadelphia, PA; 5Cooper Health Gastroenterology, Camden, NJ
Introduction: Cirrhosis is a major cause of mortality and acute care utilization placing a significant burden on healthcare systems. Our project aims to assess adherence to the guidelines set forth by the American Association for the Study of Liver Diseases (AASLD) for cirrhosis care by reviewing retrospectively collected data.
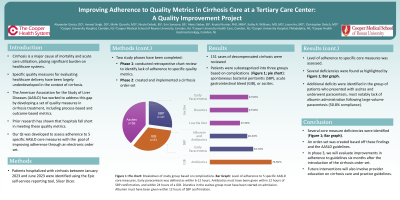
Methods: The Epic self-service reporting tool, SlicerDicer, was used to identify hospitalized cirrhosis patients between January 2023 and June 2023. ICD-10 codes for cirrhosis and its complications were used to narrow our search. Phase 1 of the study involved a retrospective chart review to identify deficiencies in cirrhosis care, specifically looking for a lack of adherence to five specific quality metrics (Table 1). In phase 2 we created and implemented a cirrhosis order-set. Phase 3 will involve post-intervention analysis for improvement in identified deficiencies.
Results: We reviewed a total of 151 cases of decompensated cirrhosis. Patients were sub-categorized by complications into three groups: spontaneous bacterial peritonitis (SBP), acute gastrointestinal bleed (GIB), or ascites. The mean age of each group was 59.2 (±) 11.98, 52.24 (±) 12.91, and 57.73 (±) 12.72, respectively. In patients with confirmed SBP (n= 41), 53.7 % had early paracentesis (within 6-12 hours), while 46.3 % were administered albumin and antibiotics within 12 hours of SBP confirmation. In patients with an acute GIB (n=51), 76.5 % had antibiotics administered within 24 hours. In decompensated patients with ascites (n=59), 37.3 % were started on a low-sodium diet, while 47.5 % had initiation of diuretics on admission. For patients decompensated with ascites, 47.5 % had early paracentesis and 66.1 % had paracentesis labs sent. For these same patients, when large-volume paracentesis (67.8 %) was performed, albumin was given in 50.8% of cases.
Discussion: In our project, we identified several core measure deficiencies. An order-set, based on AASLD guidelines, was created and implemented with the help of a multidisciplinary team. The next phase involves reassessing adherence to quality metrics after six months of utilization of this order set. Further interventions will also include provider education on practice guidelines for cirrhosis care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Garcia, DO1, Avneet Singh, DO1, Mahir Qureshi, MD1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Kathy N. Williams, MD, MS4, Jason Ho, MD5, Christopher Deitch, MD5. P1241 - Improving Adherence to Quality Metrics in Cirrhosis Care at a Tertiary Care Center: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper University Health Care, Camden, NJ; 4Cooper University Hospital, Philadelphia, PA; 5Cooper Health Gastroenterology, Camden, NJ
Introduction: Cirrhosis is a major cause of mortality and acute care utilization placing a significant burden on healthcare systems. Our project aims to assess adherence to the guidelines set forth by the American Association for the Study of Liver Diseases (AASLD) for cirrhosis care by reviewing retrospectively collected data.
Methods: The Epic self-service reporting tool, SlicerDicer, was used to identify hospitalized cirrhosis patients between January 2023 and June 2023. ICD-10 codes for cirrhosis and its complications were used to narrow our search. Phase 1 of the study involved a retrospective chart review to identify deficiencies in cirrhosis care, specifically looking for a lack of adherence to five specific quality metrics (Table 1). In phase 2 we created and implemented a cirrhosis order-set. Phase 3 will involve post-intervention analysis for improvement in identified deficiencies.
Results: We reviewed a total of 151 cases of decompensated cirrhosis. Patients were sub-categorized by complications into three groups: spontaneous bacterial peritonitis (SBP), acute gastrointestinal bleed (GIB), or ascites. The mean age of each group was 59.2 (±) 11.98, 52.24 (±) 12.91, and 57.73 (±) 12.72, respectively. In patients with confirmed SBP (n= 41), 53.7 % had early paracentesis (within 6-12 hours), while 46.3 % were administered albumin and antibiotics within 12 hours of SBP confirmation. In patients with an acute GIB (n=51), 76.5 % had antibiotics administered within 24 hours. In decompensated patients with ascites (n=59), 37.3 % were started on a low-sodium diet, while 47.5 % had initiation of diuretics on admission. For patients decompensated with ascites, 47.5 % had early paracentesis and 66.1 % had paracentesis labs sent. For these same patients, when large-volume paracentesis (67.8 %) was performed, albumin was given in 50.8% of cases.
Discussion: In our project, we identified several core measure deficiencies. An order-set, based on AASLD guidelines, was created and implemented with the help of a multidisciplinary team. The next phase involves reassessing adherence to quality metrics after six months of utilization of this order set. Further interventions will also include provider education on practice guidelines for cirrhosis care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Garcia indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Mahir Qureshi indicated no relevant financial relationships.
Nicole Debski indicated no relevant financial relationships.
Erin Sanzone indicated no relevant financial relationships.
Alexis Sieber indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Jason Ho indicated no relevant financial relationships.
Christopher Deitch indicated no relevant financial relationships.
Alexander Garcia, DO1, Avneet Singh, DO1, Mahir Qureshi, MD1, Nicole Debski, BS2, Erin Sanzone, BS2, Alexis Sieber, BS2, Krystal Hunter, PhD, MBA3, Kathy N. Williams, MD, MS4, Jason Ho, MD5, Christopher Deitch, MD5. P1241 - Improving Adherence to Quality Metrics in Cirrhosis Care at a Tertiary Care Center: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
