Sunday Poster Session
Category: Liver
P1168 - Evolving Patterns of Cirrhosis Etiology in the Era of Direct-Acting Antivirals on in a Predominately African American Population
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Ahmad Alnasarat, MD
DMC Sinai-Grace Hospital
Detroit, MI
Presenting Author(s)
Ahmad Alnasarat, MD1, Alexander N.. Minos, BSc2, Rana Khamis, BA3, Majd Khadra, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD6
1DMC Sinai-Grace Hospital, Farmington Hills, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI; 4Detroit Medical Center/Wayne State University, Detroit, MI; 5Wayne State University School of Medicine, Hazel Park, MI; 6Wayne State University, Detroit, MI
Introduction: Introduction of direct-acting antiviral therapy revolutionized HCV treatment and reduced the development of cirrhosis etiology in HCV infected individuals. It's crucial to examine local trends in cirrhosis especially in urban medical centers with respect to African American (AA) individuals compared to non-AA. The objective of this study was to determine the extent to which cirrhosis profiles of patients changed during the period when highly effective HCV antivirals were being used to cure HCV.
Methods: Using the ICD-10 codes for cirrhosis, we identified patients with a diagnosis of cirrhosis seen in 2016 as compared to 2021 (5-year interval). Patients seen in 2016 were not included in the 2021 patient dataset. The electronic medical records were used to obtain laboratory values (ALT/AST/Platelets/Albumin/Fibrospect), FibroScan, US/CT imaging, varices on EGD, and signs of decomposition (ascites, encephalopathy, and bleeding/banded varices). Consistent with our medical center demographics, the primary race was African American as compared to non-African American (72%).
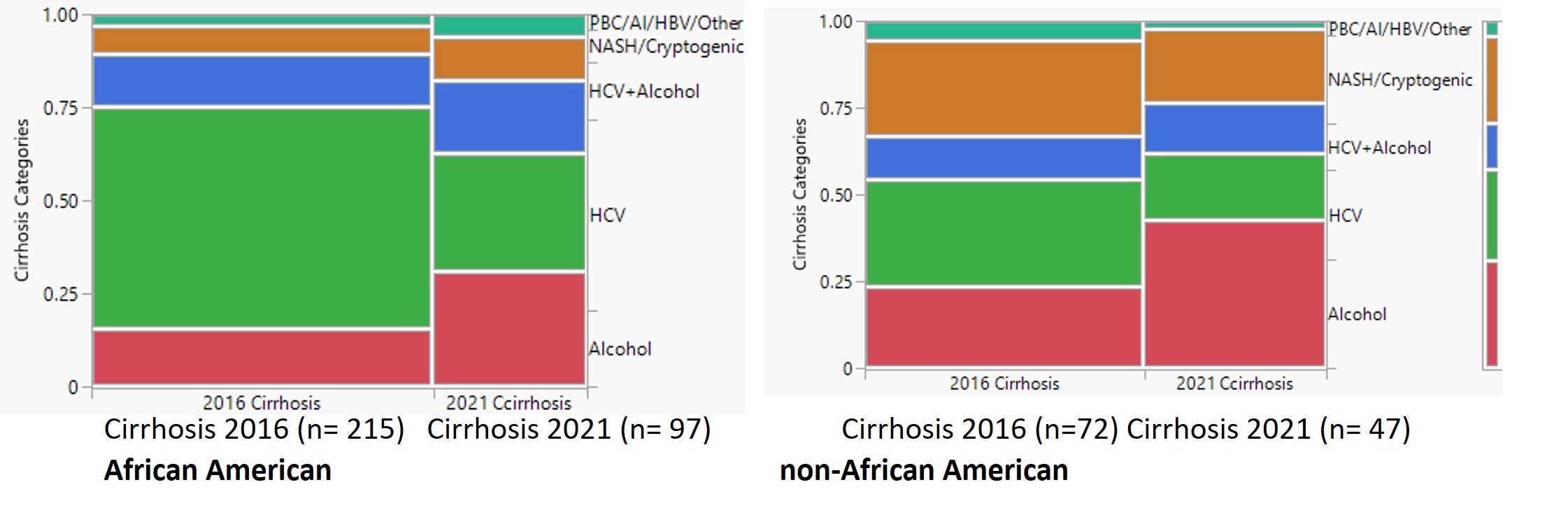
Results: The number of cirrhosis patients seen in the medical center clinics decreased from 287 in 2016 to 144 in 2021. This decline was primarily due to a decrease in patients with HCV-related cirrhosis (AA change was 59% to 32% and non-AA change was 31% to 20%; Figure 1). The proportion of patients with alcohol and NASH/Cryptogenic as risk factors subsequently increased with the decline in HCV. Non-AA patients in both eras were more likely than AA patients to have NASH/Cirrhosis. As shown in table 1 the % of patients with decompensated cirrhosis increased in 2021 as compared to 2016. Since HCV patients in 2016 had lower rates of decompensated cirrhosis (12% vs 46% for all others), the decrease in HCV patients with cirrhosis in 2021 would also account for this shift in ratio between 2016 and 2021.
Discussion: Direct antivirals led to a significant decrease in HCV-related cirrhosis and consequently total cirrhosis cases. This was especially apparent in the AAs who also have higher HCV rates as compared to non-AA individuals. Improving HCV diagnosis and treatment practices should continue to be important goals with respect to the prevention of HCC and cirrhosis. The subsequent shift to NAFLD/NASH as the etiology of cirrhosis in both AA and non-AA argues for additional attention to identifying and reducing to development of advanced fibrosis in those individuals.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmad Alnasarat, MD1, Alexander N.. Minos, BSc2, Rana Khamis, BA3, Majd Khadra, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD6. P1168 - Evolving Patterns of Cirrhosis Etiology in the Era of Direct-Acting Antivirals on in a Predominately African American Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1DMC Sinai-Grace Hospital, Farmington Hills, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI; 4Detroit Medical Center/Wayne State University, Detroit, MI; 5Wayne State University School of Medicine, Hazel Park, MI; 6Wayne State University, Detroit, MI
Introduction: Introduction of direct-acting antiviral therapy revolutionized HCV treatment and reduced the development of cirrhosis etiology in HCV infected individuals. It's crucial to examine local trends in cirrhosis especially in urban medical centers with respect to African American (AA) individuals compared to non-AA. The objective of this study was to determine the extent to which cirrhosis profiles of patients changed during the period when highly effective HCV antivirals were being used to cure HCV.
Methods: Using the ICD-10 codes for cirrhosis, we identified patients with a diagnosis of cirrhosis seen in 2016 as compared to 2021 (5-year interval). Patients seen in 2016 were not included in the 2021 patient dataset. The electronic medical records were used to obtain laboratory values (ALT/AST/Platelets/Albumin/Fibrospect), FibroScan, US/CT imaging, varices on EGD, and signs of decomposition (ascites, encephalopathy, and bleeding/banded varices). Consistent with our medical center demographics, the primary race was African American as compared to non-African American (72%).
Results: The number of cirrhosis patients seen in the medical center clinics decreased from 287 in 2016 to 144 in 2021. This decline was primarily due to a decrease in patients with HCV-related cirrhosis (AA change was 59% to 32% and non-AA change was 31% to 20%; Figure 1). The proportion of patients with alcohol and NASH/Cryptogenic as risk factors subsequently increased with the decline in HCV. Non-AA patients in both eras were more likely than AA patients to have NASH/Cirrhosis. As shown in table 1 the % of patients with decompensated cirrhosis increased in 2021 as compared to 2016. Since HCV patients in 2016 had lower rates of decompensated cirrhosis (12% vs 46% for all others), the decrease in HCV patients with cirrhosis in 2021 would also account for this shift in ratio between 2016 and 2021.
Discussion: Direct antivirals led to a significant decrease in HCV-related cirrhosis and consequently total cirrhosis cases. This was especially apparent in the AAs who also have higher HCV rates as compared to non-AA individuals. Improving HCV diagnosis and treatment practices should continue to be important goals with respect to the prevention of HCC and cirrhosis. The subsequent shift to NAFLD/NASH as the etiology of cirrhosis in both AA and non-AA argues for additional attention to identifying and reducing to development of advanced fibrosis in those individuals.
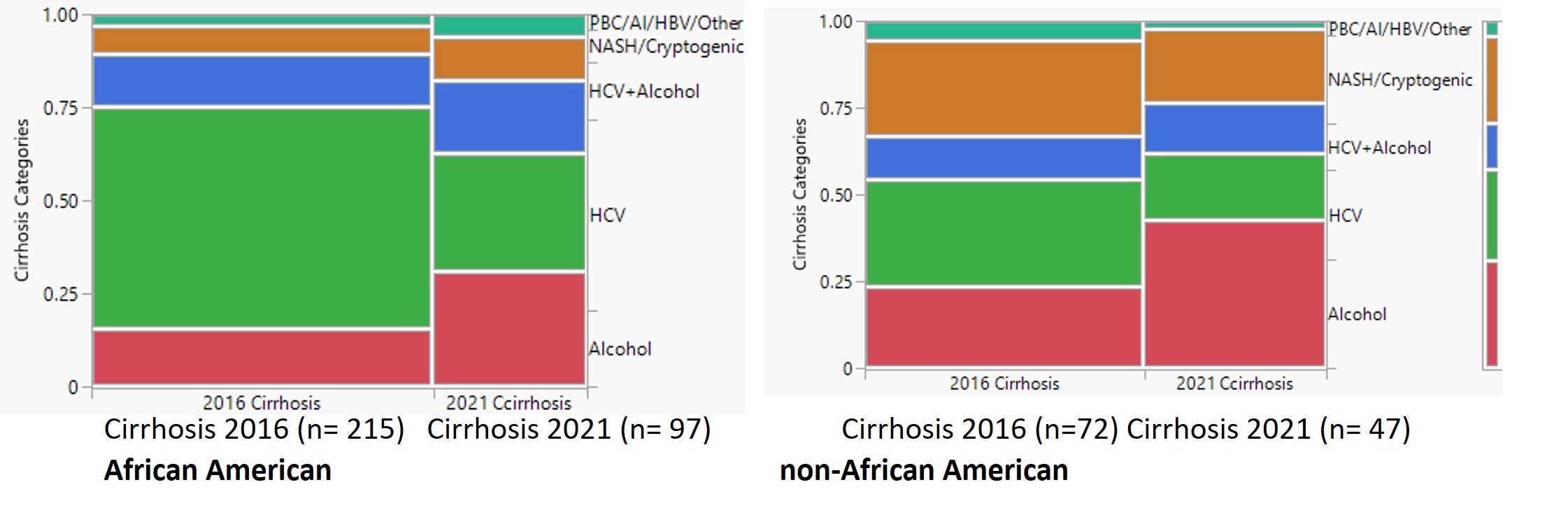
Figure: Figure 1. The mosaic graphs present the data as proportions for the number of individuals with cirrhosis seen in 2016 vs 2021 and the categories of cirrhosis. The most statistically significant difference is that AA patients in 2016 are more likely to have HCV as the risk factor than in 2021. (p<0.0005). For both AA and non-AA patients, the number of patients with cirrhosis is lower in 2021 as compared to 2016.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmad Alnasarat indicated no relevant financial relationships.
Alexander Minos indicated no relevant financial relationships.
Rana Khamis indicated no relevant financial relationships.
Majd Khadra indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Milton Mutchnick: Janssen – Grant/Research Support. Madrigal – Speakers Bureau. Salix – Grant/Research Support.
Ahmad Alnasarat, MD1, Alexander N.. Minos, BSc2, Rana Khamis, BA3, Majd Khadra, MD4, Paul H. Naylor, PhD5, Milton G. Mutchnick, MD6. P1168 - Evolving Patterns of Cirrhosis Etiology in the Era of Direct-Acting Antivirals on in a Predominately African American Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
