Sunday Poster Session
Category: Interventional Endoscopy
P1096 - Post-ERCP Balloon Dilation Haemobilia Secondary to Billroth II-Induced Biliary Stricture and Choledocholithiasis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Shu-Yen Emily Chan, MD, MSc
Weiss Memorial Hospital
Chicago, IL
Presenting Author(s)
Emily Shu-Yen Chan, MD, MSc1, Yen-Pei Chen, MD2, Natchaya Polpichai, MD1, Panisara Fangsaard, MD3, Shehzad Ali, MD1
1Weiss Memorial Hospital, Chicago, IL; 2Linkou Chang Gung Memorial Hospital, Taoyuan, Taoyuan, Taiwan; 3Bassett Medical Center, Cooperstown, NY
Introduction: Bleeding as a complication of interventional ERCP is a significant adverse event, with reported rates ranging from less than 1% to 3%. Studies indicate that endoscopic papillary balloon dilation (EPBD) may lower the risk of bleeding compared to standard sphincterotomy alone. However, EPBD is linked to a higher risk of post-ERCP pancreatitis. Here, we describe a case of complicated haemobilia and duodenal hematoma requiring transcatheter arterial embolization after EPBD.
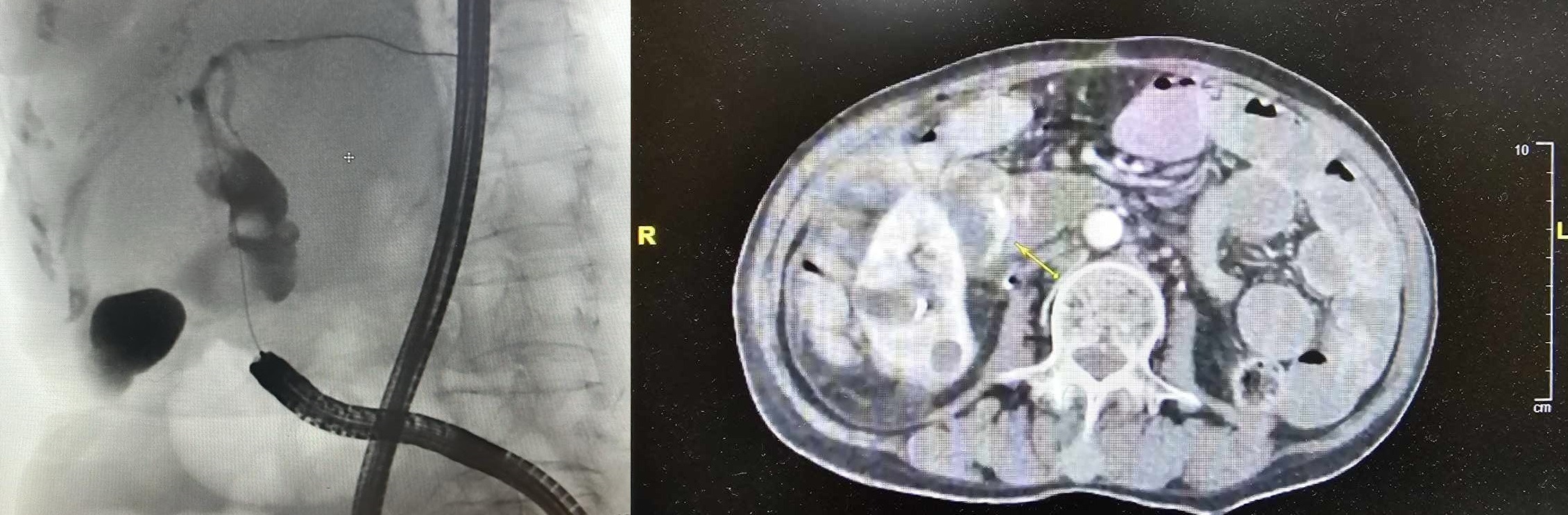
Case Description/Methods: An 82-year-old female with a history of hypertension, mitral valve prolapse, HFpEF, and a previous duodenal ulcer perforation (s/p subtotal gastrectomy and Billroth II reconstruction with choledochoduodenostomy and biliary stent placement two years ago) presented with epigastric pain and hematemesis. Five days earlier, she underwent EPBD for an asymptomatic dilated IHD, CBD/CHD and two stones removal. She was not on antiplatelets or anticoagulants. In the emergency department, she was afebrile (37.2°C) but tachycardic (121 bpm). Lab results showed anemia (Hb 6.9 g/dL), elevated liver enzymes (AST/ALT: 415/256 U/L), bilirubin (total/direct: 3.3/2.0 mg/dL), lipase (282 U/L), alkaline phosphatase (212 U/L), gamma-glutamyl transferase (338 U/L), CRP (10.4 mg/L), and lactate (7.9 mg/dL). Coagulation studies (PT/aPTT/INR) were within normal range. A CT angiogram revealed contrast extravasation at the ampulla of Vater with haemobilia and blood in the duodenum. The patient received 6U of pRBC and 2U FFP due to ongoing bloody stools. The pancreaticoduodenal arcade was embolized using a microcoil and Gelfoam cubes. Despite these interventions, her Hb remained low with continued bloody stools and fresh blood in the nasogastric tube. She received an additional 4 units of pRBC and 2 units of FFP, along with high-dose esomeprazole, antibiotics (Flomax), and tranexamic acid. She was transferred to the ICU. An upper endoscopy confirmed a duodenal ulcer at the major papilla without active bleeding.
Discussion: Billroth II anatomical alterations require accessing the papilla of Vater via the afferent loop, rendering it inverted compared to standard ERCP and increasing adverse event risks. Perforations are more frequent in Billroth II patients. Additionally, a meta-analysis of 15 randomized controlled trials showed that ERPB is slightly less effective for stone extraction and riskier for pancreatitis than endoscopic sphincterotomy, but it results in fewer infections and lower bleeding rates.
Disclosures:
Emily Shu-Yen Chan, MD, MSc1, Yen-Pei Chen, MD2, Natchaya Polpichai, MD1, Panisara Fangsaard, MD3, Shehzad Ali, MD1. P1096 - Post-ERCP Balloon Dilation Haemobilia Secondary to Billroth II-Induced Biliary Stricture and Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Weiss Memorial Hospital, Chicago, IL; 2Linkou Chang Gung Memorial Hospital, Taoyuan, Taoyuan, Taiwan; 3Bassett Medical Center, Cooperstown, NY
Introduction: Bleeding as a complication of interventional ERCP is a significant adverse event, with reported rates ranging from less than 1% to 3%. Studies indicate that endoscopic papillary balloon dilation (EPBD) may lower the risk of bleeding compared to standard sphincterotomy alone. However, EPBD is linked to a higher risk of post-ERCP pancreatitis. Here, we describe a case of complicated haemobilia and duodenal hematoma requiring transcatheter arterial embolization after EPBD.
Case Description/Methods: An 82-year-old female with a history of hypertension, mitral valve prolapse, HFpEF, and a previous duodenal ulcer perforation (s/p subtotal gastrectomy and Billroth II reconstruction with choledochoduodenostomy and biliary stent placement two years ago) presented with epigastric pain and hematemesis. Five days earlier, she underwent EPBD for an asymptomatic dilated IHD, CBD/CHD and two stones removal. She was not on antiplatelets or anticoagulants. In the emergency department, she was afebrile (37.2°C) but tachycardic (121 bpm). Lab results showed anemia (Hb 6.9 g/dL), elevated liver enzymes (AST/ALT: 415/256 U/L), bilirubin (total/direct: 3.3/2.0 mg/dL), lipase (282 U/L), alkaline phosphatase (212 U/L), gamma-glutamyl transferase (338 U/L), CRP (10.4 mg/L), and lactate (7.9 mg/dL). Coagulation studies (PT/aPTT/INR) were within normal range. A CT angiogram revealed contrast extravasation at the ampulla of Vater with haemobilia and blood in the duodenum. The patient received 6U of pRBC and 2U FFP due to ongoing bloody stools. The pancreaticoduodenal arcade was embolized using a microcoil and Gelfoam cubes. Despite these interventions, her Hb remained low with continued bloody stools and fresh blood in the nasogastric tube. She received an additional 4 units of pRBC and 2 units of FFP, along with high-dose esomeprazole, antibiotics (Flomax), and tranexamic acid. She was transferred to the ICU. An upper endoscopy confirmed a duodenal ulcer at the major papilla without active bleeding.
Discussion: Billroth II anatomical alterations require accessing the papilla of Vater via the afferent loop, rendering it inverted compared to standard ERCP and increasing adverse event risks. Perforations are more frequent in Billroth II patients. Additionally, a meta-analysis of 15 randomized controlled trials showed that ERPB is slightly less effective for stone extraction and riskier for pancreatitis than endoscopic sphincterotomy, but it results in fewer infections and lower bleeding rates.
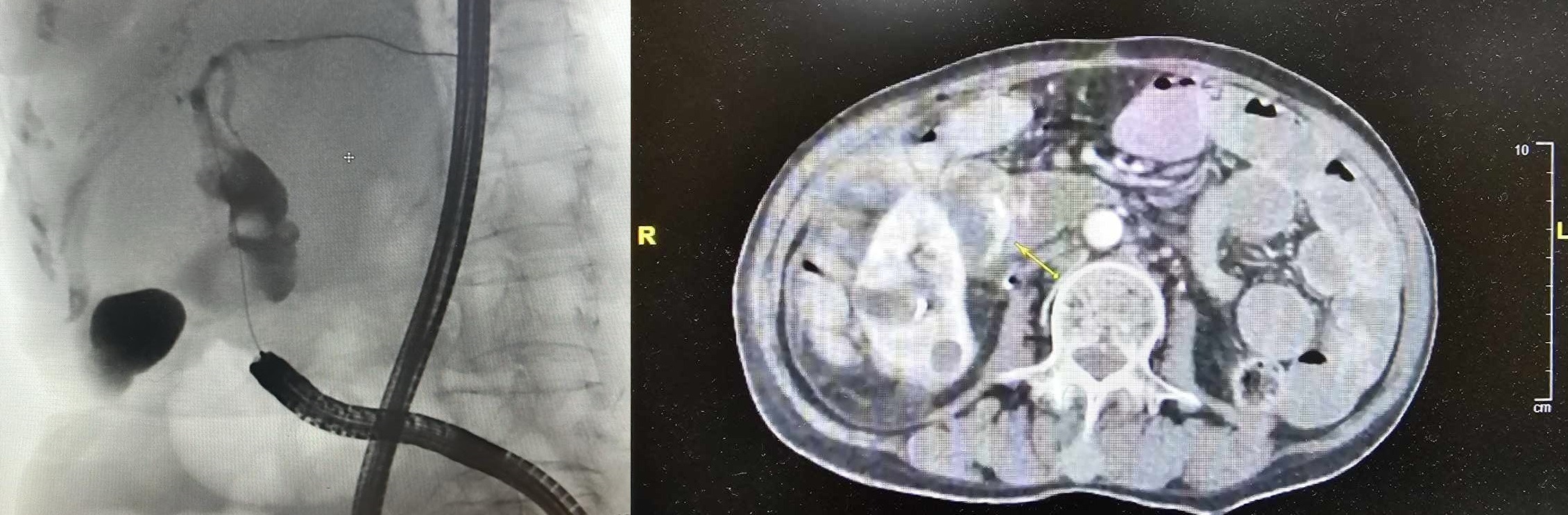
Figure: Figure 1A. ERCP 1B. CTA
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Yen-Pei Chen indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Panisara Fangsaard indicated no relevant financial relationships.
Shehzad Ali indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD, MSc1, Yen-Pei Chen, MD2, Natchaya Polpichai, MD1, Panisara Fangsaard, MD3, Shehzad Ali, MD1. P1096 - Post-ERCP Balloon Dilation Haemobilia Secondary to Billroth II-Induced Biliary Stricture and Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
