Sunday Poster Session
Category: Interventional Endoscopy
P1024 - A Comparison of Endoscopic and Surgical Gastrojejunostomy in Patients With Malignant Gastric Outlet Obstruction: A National Cohort Analysis (2016-2020)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bhanu Siva Mohan Pinnam, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Abdul Mohammed, MD2, Dushyant S. Dahiya, MD3, Saurabh Chandan, MD4, Harishankar Gopakumar, MD5, Sanket Basida, MD6, Mihir P. Shah, MD7, Hassam Ali, MD8, Manesh Kumar Gangwani, MD9, Rohit Agrawal, MD10, Hemant Mutneja, MD1, Seema Gandhi, MD1, Muhammad K. Hasan, MD2, Sumant Inamdar, MD9
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2AdventHealth, Orlando, FL; 3The University of Kansas School of Medicine, Kansas City, KS; 4CHI Health Creighton University Medical Center, Omaha, NE; 5University of Illinois College of Medicine, Bloomington, IL; 6University of Missouri School of Medicine, Columbia, MO; 7John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 8East Carolina University, Greenville, NC; 9University of Arkansas for Medical Sciences, Little Rock, AR; 10West Virginia University School of Medicine, Morgantown, WV
Introduction: Malignant gastric outlet obstruction (MGOO) is an unfortunate complication of advanced upper gastrointestinal malignancies. Historically, surgical gastrojejunostomy has been the procedure of choice to achieve enteral bypass. Recently, endoscopic techniques have gained popularity in the management of MGOO. We aimed to compare peri-procedural outcomes between surgical and endoscopic gastrojejunostomy in patients with MGOO.
Methods: The National Inpatient Sample (NIS) was queried for 2016 through 2020. The International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify adult admissions with a principal diagnosis of gastric, pancreatic, or duodenal cancer undergoing endoscopic gastrojejunostomy (EGJ) or surgical gastrojejunostomy (SGJ). The two cohorts were compared for peri-procedural adverse events.
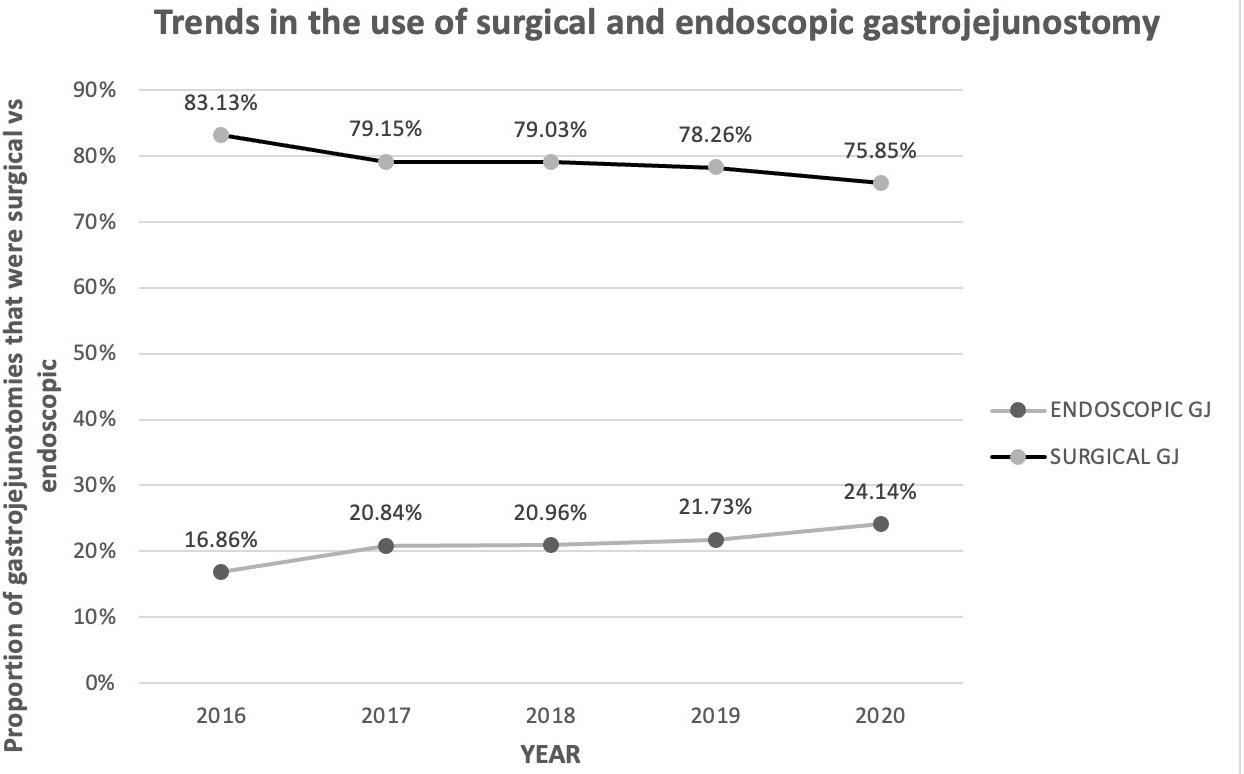
Results: Twenty thousand nine hundred thirty (20,930) hospitalizations undergoing gastrojejunostomy (16,585 SGJ and 4,345 EGJ) for MGOO were identified. The SGJ cohort had a higher proportion of patients with pancreatic cancer (36.16% vs 19.56%) and a lower proportion of patients with gastric cancer (55.16% vs 71.99%). A higher percentage of endoscopic GJs were performed in the Northeast (20.33% vs 27.66%, P< 0.001), while a smaller percentage of endoscopic GJs were performed in the South (30.56% vs. 39.52%, P < 0.001). Between the two groups, the difference in mortality rates was not significantly different [0.62, 95% CI 0.35-1.10, P =0.106), but the EGJ group had lower odds of respiratory failure [4.7% vs. 7.4%, aOR (adjusted odds ratio) 0.68, 95% CI (confidence interval) 0.48 - 0.96, P =0.032], blood transfusion [9.25% vs. 13.74%, aOR 0.63, 95% CI 0.48 – 0.82, P =0.001], and peritonitis [2.19% vs 4.5%, aOR 0.55, 95% CI 0.33-0.91, P =0.022]. The EGJ group had lesser hospitalization charges [mean $164,794 vs. $183,519, adjusted difference on regression $16,495, 95% CI $29,204 – $3,786, P =0.011], and shorter hospital stays [mean 9.88 vs. 12.56 days, adjusted difference 2.24 days, 95% CI 1.53 – 2.96 days, P < 0.001]. The use of GJ increased over five years [16.86% in 2016 to 24.14% in 2020, P-value for trend=0.002], while the use of SGJ decreased [83.13% in 2016 to 75.85% in 2020, Trend P=0.002].
Discussion: Compared to surgical GJ, endoscopic GJ is associated with lower rates of peri-procedural adverse events, hospitalization charges, and length of stay. For these reasons, EGJ should be preferred over SGJ in managing malignant gastric outlet obstruction.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Abdul Mohammed, MD2, Dushyant S. Dahiya, MD3, Saurabh Chandan, MD4, Harishankar Gopakumar, MD5, Sanket Basida, MD6, Mihir P. Shah, MD7, Hassam Ali, MD8, Manesh Kumar Gangwani, MD9, Rohit Agrawal, MD10, Hemant Mutneja, MD1, Seema Gandhi, MD1, Muhammad K. Hasan, MD2, Sumant Inamdar, MD9. P1024 - A Comparison of Endoscopic and Surgical Gastrojejunostomy in Patients With Malignant Gastric Outlet Obstruction: A National Cohort Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2AdventHealth, Orlando, FL; 3The University of Kansas School of Medicine, Kansas City, KS; 4CHI Health Creighton University Medical Center, Omaha, NE; 5University of Illinois College of Medicine, Bloomington, IL; 6University of Missouri School of Medicine, Columbia, MO; 7John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 8East Carolina University, Greenville, NC; 9University of Arkansas for Medical Sciences, Little Rock, AR; 10West Virginia University School of Medicine, Morgantown, WV
Introduction: Malignant gastric outlet obstruction (MGOO) is an unfortunate complication of advanced upper gastrointestinal malignancies. Historically, surgical gastrojejunostomy has been the procedure of choice to achieve enteral bypass. Recently, endoscopic techniques have gained popularity in the management of MGOO. We aimed to compare peri-procedural outcomes between surgical and endoscopic gastrojejunostomy in patients with MGOO.
Methods: The National Inpatient Sample (NIS) was queried for 2016 through 2020. The International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify adult admissions with a principal diagnosis of gastric, pancreatic, or duodenal cancer undergoing endoscopic gastrojejunostomy (EGJ) or surgical gastrojejunostomy (SGJ). The two cohorts were compared for peri-procedural adverse events.
Results: Twenty thousand nine hundred thirty (20,930) hospitalizations undergoing gastrojejunostomy (16,585 SGJ and 4,345 EGJ) for MGOO were identified. The SGJ cohort had a higher proportion of patients with pancreatic cancer (36.16% vs 19.56%) and a lower proportion of patients with gastric cancer (55.16% vs 71.99%). A higher percentage of endoscopic GJs were performed in the Northeast (20.33% vs 27.66%, P< 0.001), while a smaller percentage of endoscopic GJs were performed in the South (30.56% vs. 39.52%, P < 0.001). Between the two groups, the difference in mortality rates was not significantly different [0.62, 95% CI 0.35-1.10, P =0.106), but the EGJ group had lower odds of respiratory failure [4.7% vs. 7.4%, aOR (adjusted odds ratio) 0.68, 95% CI (confidence interval) 0.48 - 0.96, P =0.032], blood transfusion [9.25% vs. 13.74%, aOR 0.63, 95% CI 0.48 – 0.82, P =0.001], and peritonitis [2.19% vs 4.5%, aOR 0.55, 95% CI 0.33-0.91, P =0.022]. The EGJ group had lesser hospitalization charges [mean $164,794 vs. $183,519, adjusted difference on regression $16,495, 95% CI $29,204 – $3,786, P =0.011], and shorter hospital stays [mean 9.88 vs. 12.56 days, adjusted difference 2.24 days, 95% CI 1.53 – 2.96 days, P < 0.001]. The use of GJ increased over five years [16.86% in 2016 to 24.14% in 2020, P-value for trend=0.002], while the use of SGJ decreased [83.13% in 2016 to 75.85% in 2020, Trend P=0.002].
Discussion: Compared to surgical GJ, endoscopic GJ is associated with lower rates of peri-procedural adverse events, hospitalization charges, and length of stay. For these reasons, EGJ should be preferred over SGJ in managing malignant gastric outlet obstruction.
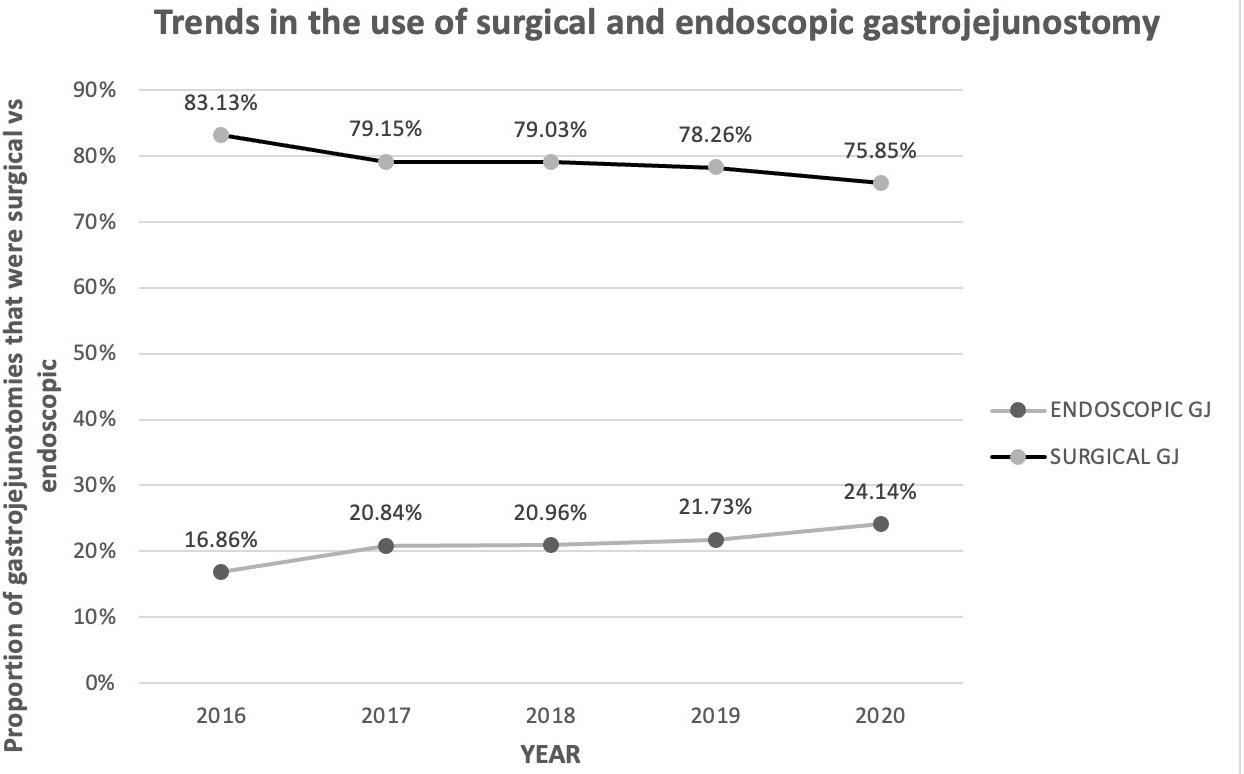
Figure: Figure: Trend in the use of surgical vs endoscopic gastrojejunostomy in the treatment of malignant gastric outlet obstruction, 2016 to 2020
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Pius Ojemolon indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Harishankar Gopakumar indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Mihir Shah indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Hemant Mutneja indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Muhammad Hasan: Boston Scientific – Consultant. microtech – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Sumant Inamdar indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Abdul Mohammed, MD2, Dushyant S. Dahiya, MD3, Saurabh Chandan, MD4, Harishankar Gopakumar, MD5, Sanket Basida, MD6, Mihir P. Shah, MD7, Hassam Ali, MD8, Manesh Kumar Gangwani, MD9, Rohit Agrawal, MD10, Hemant Mutneja, MD1, Seema Gandhi, MD1, Muhammad K. Hasan, MD2, Sumant Inamdar, MD9. P1024 - A Comparison of Endoscopic and Surgical Gastrojejunostomy in Patients With Malignant Gastric Outlet Obstruction: A National Cohort Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
