Sunday Poster Session
Category: Interventional Endoscopy
P1031 - Anterior versus Posterior Approach in Peroral Endoscopic Myotomy (POEM) in Patients with Achalasia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdul-Rahman F. Diab, MD
University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME
Ocala, FL
Presenting Author(s)
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Peroral endoscopic myotomy (POEM) is a well-established procedure for the management of achalasia. POEM can be performed using either an anterior or posterior approach. However, there is limited knowledge about the differences between these two approaches in terms of safety, efficacy in treating achalasia, and the risk of gastroesophageal reflux disease (GERD). A prevalent assumption is that the anterior approach may lead to a lower incidence of GERD. This study aimed to compare these two approaches using a pairwise meta-analysis.
Methods: A systematic literature review was conducted following PRISMA guidelines to identify articles that directly compare the anterior and posterior approaches of POEM in achalasia management. A random effects model was used for the analysis, with odds ratios for dichotomous data and mean differences for continuous data.
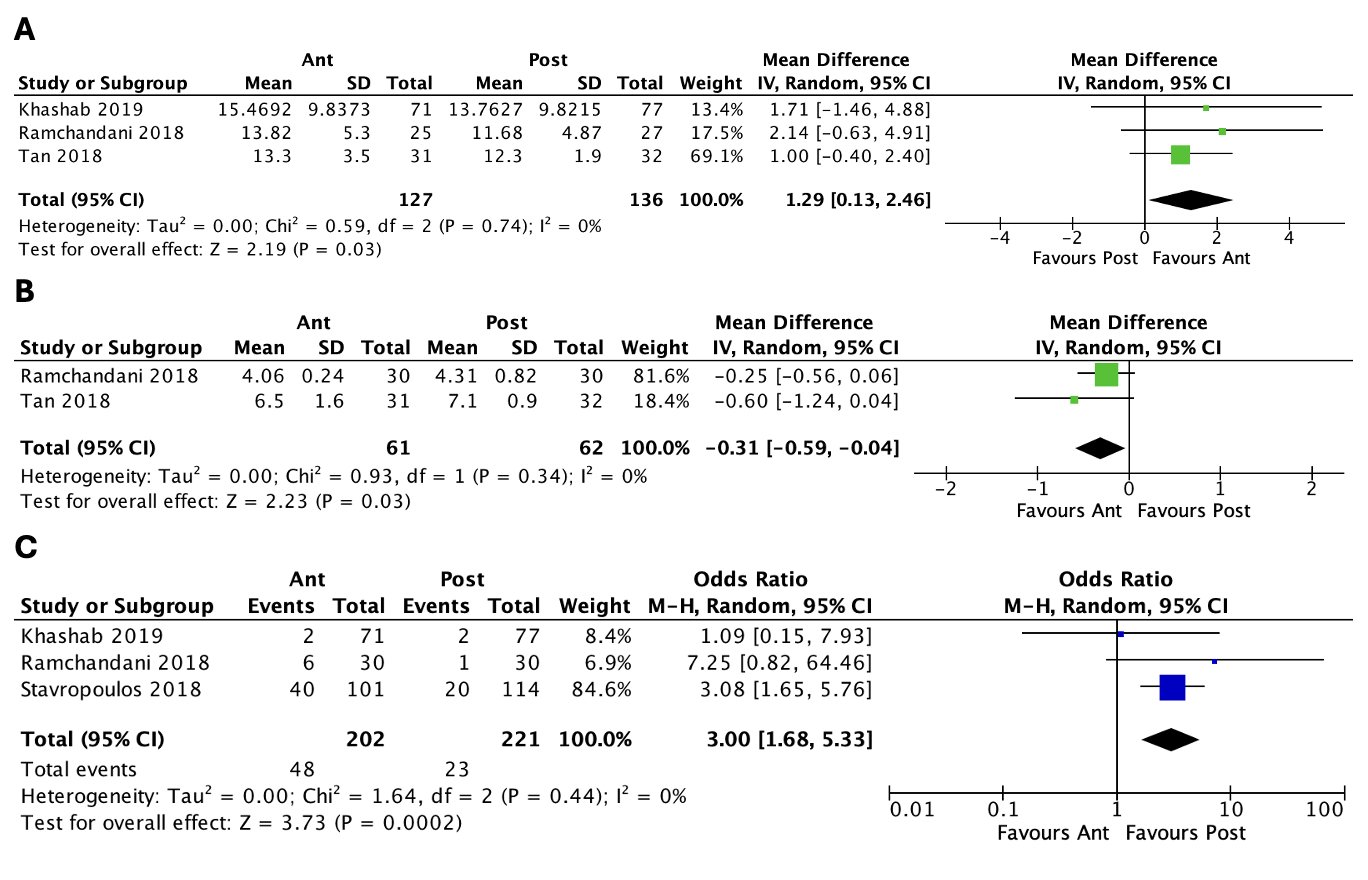
Results: Eight studies were included in the analysis. No significant differences were found in efficacy-related outcomes, including clinical success (Eckardt score < 3), manometric remission (IRP < 14), Eckardt score, and integrated relaxing pressure (IRP). Regarding GERD-related outcomes, although no significant differences were found in GERD (diagnosed by symptom scores, pH monitoring, or endoscopy revealing esophagitis) and proton pump inhibitor (PPI) use, the mean lower esophageal sphincter (LES) pressure was significantly higher in the anterior group. For perioperative outcomes, no significant difference in procedural time was observed, but the length of stay (LOS) was significantly shorter in the anterior group. Regarding safety-related outcomes, no significant differences were found in total adverse events, perforations, pneumothorax, and pneumomediastinum; however, inadvertent mucosotomies were significantly more frequent in the anterior group. For a detailed and quantitative description of the results, please refer to the accompanying table.
Discussion: This study suggests generally comparable outcomes between the anterior and posterior approaches of POEM. Although LES pressures were higher in the anterior group, this did not correlate with a decreased incidence of GERD or reflux esophagitis. Inadvertent mucosotomies were more frequent in the anterior group, but the LOS was shorter. To date, there is no evidence to suggest the superiority of one approach over the other. Further studies are needed to optimize the technique.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1031 - Anterior versus Posterior Approach in Peroral Endoscopic Myotomy (POEM) in Patients with Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Peroral endoscopic myotomy (POEM) is a well-established procedure for the management of achalasia. POEM can be performed using either an anterior or posterior approach. However, there is limited knowledge about the differences between these two approaches in terms of safety, efficacy in treating achalasia, and the risk of gastroesophageal reflux disease (GERD). A prevalent assumption is that the anterior approach may lead to a lower incidence of GERD. This study aimed to compare these two approaches using a pairwise meta-analysis.
Methods: A systematic literature review was conducted following PRISMA guidelines to identify articles that directly compare the anterior and posterior approaches of POEM in achalasia management. A random effects model was used for the analysis, with odds ratios for dichotomous data and mean differences for continuous data.
Results: Eight studies were included in the analysis. No significant differences were found in efficacy-related outcomes, including clinical success (Eckardt score < 3), manometric remission (IRP < 14), Eckardt score, and integrated relaxing pressure (IRP). Regarding GERD-related outcomes, although no significant differences were found in GERD (diagnosed by symptom scores, pH monitoring, or endoscopy revealing esophagitis) and proton pump inhibitor (PPI) use, the mean lower esophageal sphincter (LES) pressure was significantly higher in the anterior group. For perioperative outcomes, no significant difference in procedural time was observed, but the length of stay (LOS) was significantly shorter in the anterior group. Regarding safety-related outcomes, no significant differences were found in total adverse events, perforations, pneumothorax, and pneumomediastinum; however, inadvertent mucosotomies were significantly more frequent in the anterior group. For a detailed and quantitative description of the results, please refer to the accompanying table.
Discussion: This study suggests generally comparable outcomes between the anterior and posterior approaches of POEM. Although LES pressures were higher in the anterior group, this did not correlate with a decreased incidence of GERD or reflux esophagitis. Inadvertent mucosotomies were more frequent in the anterior group, but the LOS was shorter. To date, there is no evidence to suggest the superiority of one approach over the other. Further studies are needed to optimize the technique.
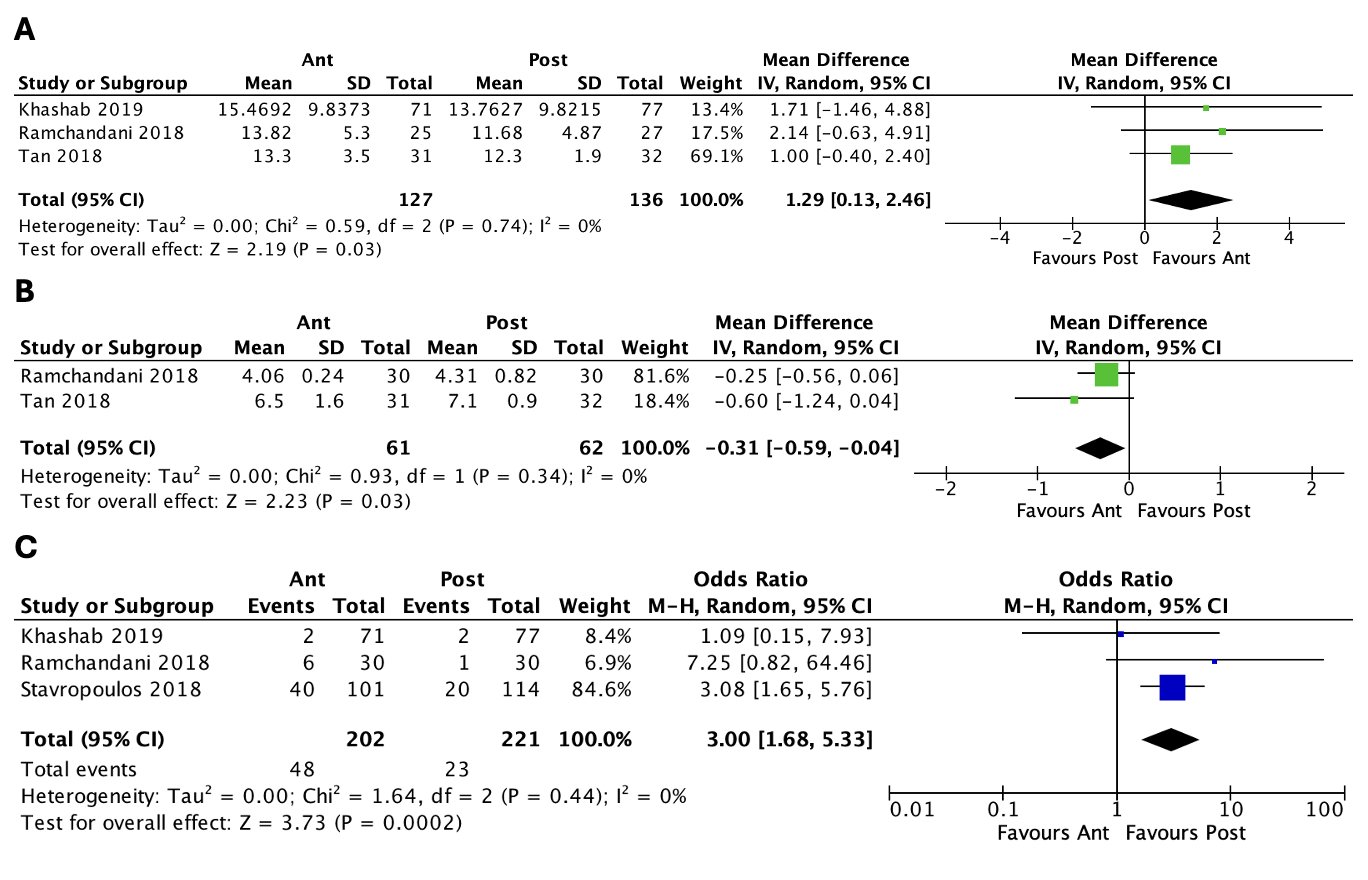
Figure: Lower esophageal sphincter pressure (A), length of stay (B), and mucosotomy (C).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdul-Rahman Diab indicated no relevant financial relationships.
Joseph Sujka indicated no relevant financial relationships.
Kathleen Mattingly indicated no relevant financial relationships.
Angelica McCaskey indicated no relevant financial relationships.
Abdullah Elnaji indicated no relevant financial relationships.
Salvatore Docimo indicated no relevant financial relationships.
Christopher DuCoin indicated no relevant financial relationships.
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P1031 - Anterior versus Posterior Approach in Peroral Endoscopic Myotomy (POEM) in Patients with Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
