Sunday Poster Session
Category: IBD
P0945 - Readmission Rates in the Inflammatory Bowel Disease Population After Coronary Artery Bypass Grafting: A Nationwide Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Prabhat Kumar, MD
Cleveland Clinic Foundation
Richmond, VA
Presenting Author(s)
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Ashraf Almomani, MD2, Ankit Agrawal, MD1, Omar Saab, MD1, Sanya Chandna, MD1, Manik Aggarwal, MBBS3, Stephen J. Bickston, MD, FACG4
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Florida, Weston, FL; 3Mayo Clinic, Rochester, MN; 4Virginia Commonwealth University Health System, Richmond, VA
Introduction: Patients with inflammatory bowel disease (IBD) are at increased risk for cardiovascular diseases and gastrointestinal diseases, including those necessitating coronary artery bypass grafting (CABG). However, limited data exist on the readmission rates and causes of readmission in IBD patients following CABG. This study aims to evaluate the readmission rates and identify key predictors of readmission in IBD patients post-CABG using the Nationwide Readmissions Database (NRD).
Methods: A retrospective cohort study was conducted using the NRD to identify adult patients who underwent CABG between January 1, 2016, and November 31, 2020. Patients with a diagnosis of IBD (Crohn's disease & ulcerative colitis) were identified using the International Classification of Diseases, 10th revision, Clinical Modification coding system. The primary outcome was the 30-day readmission rate post-CABG. Secondary outcomes included causes of readmission and predictors of readmission. Statistical analysis was performed using logistic regression to adjust for potential confounders. Multivariate and Survival analyses were performed to calculate respective unadjusted/adjusted odds and hazard ratios.
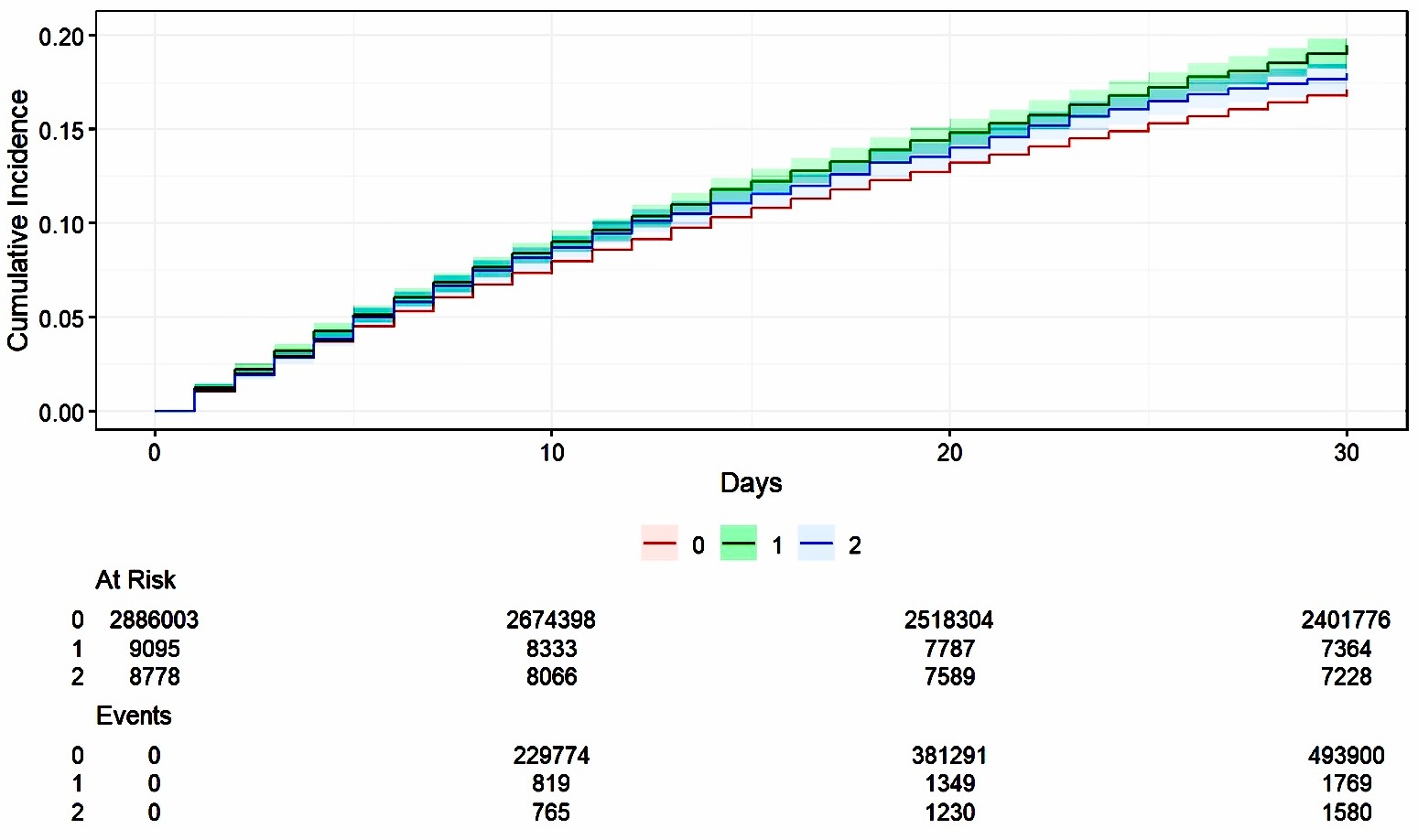
Results: Out of 5.2 million patients discharged after CABG surgery, 42,573 had IBD (16,248 UC; 17,360 CD). Readmission rates were 19% for UC and 18% for CD. The most common causes of readmission in IBD patients were sepsis, acute kidney injury, and heart failure. The cumulative incidence of readmission was higher in UC compared to CD and non-IBD patients [graph 1]. Significant predictors of readmission included acute liver failure (UC, p=0.019), blood transfusions (p< 0.01), and mesenteric ischemia (p=0.05) [Table 1]. The IBD cohort had higher readmission rates for acute liver failure, blood transfusion, and mesenteric ischemia compared to the non-IBD cohort (p< 0.01). Rates of venous thromboembolism did not differ between IBD and non-IBD groups.
Discussion: IBD patients undergoing CABG have a significantly higher 30-day readmission rate compared to non-IBD patients. The primary reasons for readmission are infections, cardiac/renal complications, and gastrointestinal issues. These findings highlight the need for targeted strategies to reduce readmission rates in this high-risk population, such as enhanced perioperative management and close post-discharge monitoring.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Ashraf Almomani, MD2, Ankit Agrawal, MD1, Omar Saab, MD1, Sanya Chandna, MD1, Manik Aggarwal, MBBS3, Stephen J. Bickston, MD, FACG4. P0945 - Readmission Rates in the Inflammatory Bowel Disease Population After Coronary Artery Bypass Grafting: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Florida, Weston, FL; 3Mayo Clinic, Rochester, MN; 4Virginia Commonwealth University Health System, Richmond, VA
Introduction: Patients with inflammatory bowel disease (IBD) are at increased risk for cardiovascular diseases and gastrointestinal diseases, including those necessitating coronary artery bypass grafting (CABG). However, limited data exist on the readmission rates and causes of readmission in IBD patients following CABG. This study aims to evaluate the readmission rates and identify key predictors of readmission in IBD patients post-CABG using the Nationwide Readmissions Database (NRD).
Methods: A retrospective cohort study was conducted using the NRD to identify adult patients who underwent CABG between January 1, 2016, and November 31, 2020. Patients with a diagnosis of IBD (Crohn's disease & ulcerative colitis) were identified using the International Classification of Diseases, 10th revision, Clinical Modification coding system. The primary outcome was the 30-day readmission rate post-CABG. Secondary outcomes included causes of readmission and predictors of readmission. Statistical analysis was performed using logistic regression to adjust for potential confounders. Multivariate and Survival analyses were performed to calculate respective unadjusted/adjusted odds and hazard ratios.
Results: Out of 5.2 million patients discharged after CABG surgery, 42,573 had IBD (16,248 UC; 17,360 CD). Readmission rates were 19% for UC and 18% for CD. The most common causes of readmission in IBD patients were sepsis, acute kidney injury, and heart failure. The cumulative incidence of readmission was higher in UC compared to CD and non-IBD patients [graph 1]. Significant predictors of readmission included acute liver failure (UC, p=0.019), blood transfusions (p< 0.01), and mesenteric ischemia (p=0.05) [Table 1]. The IBD cohort had higher readmission rates for acute liver failure, blood transfusion, and mesenteric ischemia compared to the non-IBD cohort (p< 0.01). Rates of venous thromboembolism did not differ between IBD and non-IBD groups.
Discussion: IBD patients undergoing CABG have a significantly higher 30-day readmission rate compared to non-IBD patients. The primary reasons for readmission are infections, cardiac/renal complications, and gastrointestinal issues. These findings highlight the need for targeted strategies to reduce readmission rates in this high-risk population, such as enhanced perioperative management and close post-discharge monitoring.
Figure: Cumulative incidence of readmissions in patients with and without IBD who underwent CABG on the index admission.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Omar Saab indicated no relevant financial relationships.
Sanya Chandna indicated no relevant financial relationships.
Manik Aggarwal indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Ashraf Almomani, MD2, Ankit Agrawal, MD1, Omar Saab, MD1, Sanya Chandna, MD1, Manik Aggarwal, MBBS3, Stephen J. Bickston, MD, FACG4. P0945 - Readmission Rates in the Inflammatory Bowel Disease Population After Coronary Artery Bypass Grafting: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
